
Executive Summary
Evidence-based nutrition interventions exist that can positively impact maternal and child nutrition. They also can significantly reduce mortality, if sufficient programmatic coverage is achieved (Bhutta et al. 2013). However, health care workers (HCW) are not consistently tasked to promote these interventions, and if tasked, they often receive little or insufficient training. The importance of training is echoed throughout the literature and program documents; however, the actual process of how the trainings are conducted (length, depth, content, organization, etc.) is often not carefully considered, documented, reported, or evaluated. Much of what is known about the training process for nutrition is based on qualitative feedback and lessons learned found in project documents.
Given the need to strengthen nutrition services within health systems, SPRING has explored the advantages and disadvantages of two approaches that we use in Haiti for rolling out trainings on infant and young child feeding (IYCF) and nutrition assessment, counseling, and support (NACS) for health facility staff. Specifically, we looked at an on-the-job (OJT) training methodology and the more traditional approach of workshop-style trainings. We prepared a modular training package, which could be used for either approach, and presented the two training options to in-house master trainers and health facility managers. Each of the seven participating facilities selected the approach it felt was most appropriate for its facility. SPRING took responsibility for training the master trainers (MT) but provided relatively little additional support to facilities for the rollout of the training to designated facility staff.
Recognizing the gap in evidence related to effective training approaches and the extensive resources that are invested in trainings, SPRING set out to explore the advantages and disadvantages of the approaches employed by the facilities to roll out trainings. Primary data for this study were collected before and one year after the training of trainers (TOT) in January-February of 2014 and 2015, using multiple methods, including pre- and post-training tests, structured interviews, and self-administered surveys with MTs, facility managers, and health providers; in-depth interviews with health facility staff (managers, trainers, and providers); direct, systematic observation of client-provider interactions; and a final debrief with health facility staff. Due to time and budgetary constraints, there was no control group and we collected relatively small samples.
Although the two training approaches were designed to be quite different, ultimately, the approaches that the health facilities selected and followed were fewer than originally anticipated. For instance, all trainings were conducted on-site, in the facilities, thus eliminating many expenses often associated with traditional cascade trainings (rental of offsite trainings, per diem, travel, etc.). Also, all trainers were staff members working in the same facilities, which eliminated the cost of external facilitation. Holding the trainings in the facilities also meant that all trainees had the potential to receive regular coaching immediately following the training. Training on-site had its advantages (e.g., increased participation), but also resulted in a greater risk of the trainees being called away from the training to perform work duties and disrupting the learning process. Trainers identified this as a major challenge.
Improvements were impressive under both training approaches in terms of the trainees’ ability to carry out nutrition assessments according to standards. Although this change cannot be attributed to the training alone, much can be learned from this research.
Satisfaction appeared to be higher and observed nutrition assessment and counseling have improved more in facilities where the modular training approach was followed. However, trainees from the facilities following the traditional approach were more likely to mention a range of benefits from the training than those from the other facilities. Those benefits include increased knowledge, improved ability to conduct nutrition assessment and counseling, and strengthened job credentials for future job opportunities.
Unexpectedly, but perhaps not surprising given the severe human resource shortages that many health facilities face in Haiti, HCWs were sometimes selected out of convenience or availability rather than for more strategic reasons, such as the relevance of nutrition training to their job performance. Those HCWs who might have been best placed to put knowledge into practice or to make significant shifts in routine nutrition services often could not be spared and, therefore, did not always participate in the training. This was observed in the traditional and modular training approach facilities but more so in the traditional training facilities where colleagues and patients more acutely felt the absence of multiple HCWs for a larger block of time over a concentrated two-week period.
Although differences were somewhat fewer than expected, the findings indicate that trainees liked the modular training approach better, and it carried less of a financial or opportunity cost for facilities and facility staff. While all trainings did occur on-site (in the facilities) and provided some amount of opportunity to put knowledge into practice, where the modular training approach was followed, trainees had increased opportunities for more immediate practice of new skills and reinforcement of knowledge attained. Staff members’ enrollment also was higher in modular training facilities because they did not have to miss a large block of work time to participate.
Some unique challenges also appeared in the modular approach. In particular, it was difficult to ensure that trainees attended all sessions of the modular training, and it was difficult to ensure attendance over the entire course of numerous sessions given staff rotations, turnover, and annual leave.
Given the realities on the ground in Haiti, including limited financial resources and human resources— both within the SPRING/Haiti team and at the health facilities—all facilities experienced similar challenges that affect the effectiveness of the nutrition services training. Given recent changes in national protocols, certain staff members are now expected to add NACS services to their routine services. However, they are already overworked. Without additional staff or staff specifically dedicated to assessing nutritional status, providing nutrition counseling, or referring clients to nutrition support services, it may be challenging, if not impossible, to achieve full coverage of NACS services at the facility level.
Based on these findings, we feel strongly that strengthening the overall systems to better integrate nutrition services would have the greatest impact. To do this, ministries of health would need to define and implement—
- nutrition standards of care and priority elements for each level of the health system
- human resources necessary – quantity and levels – for providing those standards of care at each level
- specific training needs (content, duration, pre-service vs. in-service vs. refresher, methodology) of each cadre or role within health facilities at each level)
- a data-driven quality improvement (QI) approach to service delivery that continuously identifies and addresses barriers to the delivery of the standards of care.
We recommend that governments and projects take the following actions, if and when in-service training is deemed appropriate. These steps will help to cautiously amplify the use of modular training approaches with shorter training sessions rolled out over an extended period of time.
- Take proactive steps to orient, encourage ownership of, and gain support from facility managers to ensure the proper selection of trainers and trainees and to increase the material and “moral” support often needed for a successful training. This could be accomplished through more in-depth and strategic orientations for facility or unit managers (directors and administrators).
- Before a TOT, it is important to engage facility managers in a workshop to develop a vision for improved nutritional support services and to teach them to use data to monitor changes in performance of nutritional service-related tasks.
- Prioritize documentation of training processes and analysis comparing various approaches. Without great effort or cost, process monitoring and analysis can be integrated into routine monitoring (using existing information systems) or supervision.
- Be strategic in the selection of trainers and trainees both in terms of applicability of content to daily work (i.e., those who work in prenatal, pediatric, or HIV units) and motivation/interest in the topic.
- Train HCWs in what they can realistically do given existing equipment and infrastructure and time/workload.
- Consider carefully the timing of trainings (days of the week and hours of the day), so they are least disruptive to client flow and the normal functions of HCWs.
- Emphasize the experiential learning cycle more during future TOT, encouraging trainers to build on what trainees already know and providing adequate time to practice counseling skills during the trainings.
- Ensure the provision of an adequate space for the training, a stand for flip charts, a projector, and an energy source to run the projector.
- Adjust the workload of trainers (health facility staff) or other facility staff to allow time for adequate preparation for, implementation of, and follow-up to the training (i.e., coaching). The latter is a valuable aspect of the OJT approach, which overworked trainers often neglect.
- Incentivize trainees to participate in all training sessions for the entirety of each session. This could be done by having participation in trainings be reflected (and valued) in their performance reviews.
Introduction
Background
In 2012, USAID invited SPRING to Haiti. After Somalia and Afghanistan, Haiti suffers from the highest rates of hunger in the world. According to Haiti’s most recent Demographic and Health Survey (DHS), only 10 percent of breastfed and 15 percent of non-breastfed children 6–23 months are fed in accordance with the infant and young child feeding (IYCF) practices (MSPP, IHE, and ICF International 2013). Moreover, 22 percent of children are stunted, which indicates chronic malnutrition, and 11 percent are underweight (MSPP, IHE, and ICF International 2013). Demonstrating widespread micronutrient deficiencies, 65 percent of babies 6–59 months and almost 50 percent of women 15–49 years suffer from anemia. Haiti’s environmental vulnerability has presented significant challenges to effect sustainable nutritional solutions. Decades of deforestation and the devastation that the 2010 earthquake, Tropical Storm Isaac, and Hurricane Sandy caused have presented further challenges by causing significant flooding and contributing to loss of harvests (WFP 2014; Crist 2006).
In Haiti, we were asked to focus on supporting 17 tertiary health facilities provided as part of the Manman ak Timoun Ansante (Healthy Mothers and Children) initiative. The initiative began in 2010 and was led by the Ministère de Santé Publique et de la Population (MSPP), with support from the Pan American Health Organization and the Canadian International Development Agency. The initiative, which ended in 2013, provided high-quality care to pregnant women and children under age five. We are building on that delivery platform to strengthen the capacity of facility-based providers to deliver nutrition assessment, counseling, and support (NACS) services using modular trainings and quality improvement methods.
Recognizing the need for training health care workers (HCW), the gap in knowledge related to effective training approaches (see Annex 1 for a summary of the evidence), and the extensive resources that are invested in trainings, we set out to explore the effects, strengths, and weaknesses of SPRING’s approaches to nutrition-related trainings of health facility staff in Haiti. The trainings were rolled out with limited additional support and in a context that was often less than supportive of change in service delivery practices.
Research Questions
Through this research we looked at two approaches: occasional training sessions (short modules rolled out over many days/week) and a more traditional approach of 5–10 consecutive days for 4–8 hours per day. Key research questions included—
- How receptive have HCWs been to the trainings, depending on the training approach used?
- To what extent has the experiential learning cycle (ELC) been followed by master trainers (MT)? Does this depend on the training approach used?
- What are the costs of rolling out the training using the different approaches?
- What knowledge has been gained by HCWs; does it vary depending on the training approach used?
- Have nutrition services changed as a result of the trainings? How do changes vary depending on the training approach used?
Methods
As presented in Table 1, primary data for this study were collected before (January 2014) and one year after the training of trainers (TOT) (January – February 2015) using multiple methods, including pre- and post-training tests, structured interviews, and self-administered surveys with MTs, facility managers, and health providers; in-depth interviews with health facility staff (managers, trainers, and providers); direct, systematic observation of client-provider interactions; and a final debrief with health facility staff. We had planned on conducting a test of knowledge retention for trainees during the follow-up facility assessments; however, the MSPP requested that this activity be dropped from the research because HCWs would be unduly stressed by and would negatively perceive the assessments. SPRING staff members’ experiences and routine tracking were used to supplement, explain, or corroborate findings.
The Institutional Review Board of JSI Research & Training Institute (JSI) and the Comité National de Bioéthique of the MSPP approved for ethical review the protocol and tools for data collection. All data collection activities requested consent and took steps to ensure confidentiality and protect respondents from any negative repercussions.
Table 1. Data collection methods and sample sizes at each time point
| Data Source | Baseline | Follow-up |
|---|---|---|
| Register reviews | ||
| Observation of client-provider interactions*** | ||
| Interview with facility and unit managers | 28 | 25* |
| Prenatal care | -- | 120 |
| Pediatric care | 179 | 150 |
| HIV and AIDS** | 1022 | 1227 |
| Prenatal care | 122 | 38 |
| Pediatric care | 75 | 45 |
| HIV and AIDS | 64 | 40 |
| Pre- and post-training tests of master trainers | 22 | NA |
| Pre- and post-training tests of trainees | 149 | NA |
| In-depth qualitative interviews with master trainers | NA | 16 |
| In-depth qualitative interviews with trainees | NA | 31 |
* The facility manager of Hôpital la Providence des Gonaives was not available during data collection, so the data collection team could not obtain this information.
** Data from HIV and AIDS units were collected for all clients using the EMR system and were only made available in five of the seven health facilities included in this research.
*** Sample sizes at baseline and follow-up for each unit and facility type (training approach) were as follows: Prenatal units: Traditional (42/12), Modular (62/21), Abbreviated (20/5); Pediatric units: Traditional (48/23), Modular (27/22), Abbreviated (9/7); HIV units: Traditional (25/21), Modular (39/19), Abbreviated (10/11)
Data were analyzed in Microsoft Excel and are presented by the approach to rolling out the training that was followed. Since the rollout of the training in one facility (Hôpital Maternité Isaie Jeanty) was ultimately carried out following an abbreviated approach (see section III. C. below), findings from this facility are presented separately. Data for individual health facilities are available upon request.
The findings from this assessment should be useful for USAID, governments, and implementing partners interested in promoting or strengthening NACS services at the facility level to reach all ages, both men and women, as well as people who are HIV-positive and HIV-negative.
Intervention
In Haiti, our primary focus has been on training HCWs to strengthen the integration of NACS into existing health programs. To do this, we used two distinct, but complementary, training packages. With a growing recognition of the importance of nutrition among mothers and children in the 1,000 days from a child’s conception through her child’s 2nd birthday, as well as the need for nutrition counseling, On-the-Job Training for Health Workers: Infant and Young Child Feeding Counseling (Formation sur Site pour le Prestataires de Soins: Assistance Conseil sur l'Alimentation du Nourrisson et du Jeune Enfant) was developed with the support of SPRING, in coordination with the MSPP. It was intended to complement Nutrition Assessment, Counseling, and Support: Provisional Facilitator’s Guide for Training Facility-Based Health Workers (Evaluation, conseil et soutien en nutrition: Guide provisoire du facilitateur pour la formation des prestataires de soins dans les institutions sanitaires), which was developed for Haiti, with support from the Food and Nutrition Technical Assistance Project (FANTA III).
Both training packages were designed for modular implementation, covering training techniques and the following technical topics:
- Why IYCF matters
- Recommended IYCF practices: breastfeeding
- How to breastfeed
- Common situations that can affect breastfeeding
- Common breastfeeding difficulties: symptoms, prevention, and "what to do"
- Complementary feeding
- IYCF in the context of HIV
- Feeding the sick child
- Women’s nutrition
- Nutritional needs of people living with HIV (PLHIV)
- Nutrition assessment (physical)
- Nutrition assessment (biochemical)
- Appetite test
- Criteria for treatment of malnutrition
- Products for treatment of malnutrition
- How to counsel
- How to develop nutrition action plans
- How to conduct group education
We support 17 tertiary health care facilities in nine departments. These facilities were selected in collaboration with USAID and the MSPP. This operations research focuses on the following seven health facilities where SPRING began operating in November 2013:
- Hôpital Maternité Isaie Jeanty, West Department
- Hôpital Eliazar Germain, West Department
- Hôpital Notre Dame de Petit Goâve, West Department
- Hôpital Sainte Thérèse de Hinche, Center Department
- Hôpital la Providence des Gonaives, Artibonite Department
- Hôpital de Fort Liberté, Northeast Department
- Centre Medico Social de Ouanaminthe, Northeast Department
We trained three – four staff members from each facility to serve as MTs charged with training approximately 25 additional staff from their respective health facilities. The TOT, which included 53 hours of modules, was conducted over 6.5 days to allow for practical exercises. It included 11.5 hours on training techniques and 42.5 hours on the technical content. In addition, each MT was provided with the following materials:
- IYCF Trainer's Manual
- IYCF Participant's Manual (25 copies)
- IYCF training slides
- Video on early initiation of breastfeeding, breastmilk expression, and cup feeding
- Video “Latch 1,2,3” (with a hard copy of the French translation)
- IYCF counseling cards (bound and laminated)
- IYCF brochures (two different brochures)
- IYCF posters
- NACS Trainer’s Manual
- NACS Participant’s Manual (25 copies)
- NACS training slides
- NACS counseling cards (bound and laminated)
- Flip charts
- Markers
The TOT culminated in MTs developing action plans for rolling out the training in their respective health facilities. We proposed two distinct approaches for rolling out the training: (1) a more traditional workshop-style training conducted for a short but intensive period of time (approximately 5–10 days) and (2) a modular training approach designed to be rolled out to facility staff using a series of concise and practical two- to three-hour modules conducted one – two times per week at the facility over approximately 12 weeks. The approach was decided in consultation with health facility managers or directors.
In addition, SPRING supported MTs in conducting a sensitization meeting and in carrying out the trainings following the approach selected, covering the cost of food and print materials for the training. We visited each facility at least once in the year following the TOT to check on progress, to discuss challenges, and to propose possible solutions. We also coordinated with the MSPP nutrition focal persons to engage them in following up on the training at least once during the same time period.
Findings
Health Facilities
The number of staff members employed by the facilities varies considerably by facility and by facility type or training approach (see Table 2). On average, all three priority units of facilities where the traditional approach to rolling out the training was used had a greater number of nurses, midwives, and nursing assistants in their pediatric and HIV units than did facilities where the modular training approach was used. The fact that none of the units in any of the facilities reported having a nutritionist on staff is also worthy of note. Limited and variable human resources may have affected impact, particularly related to counseling, since this is one service that often is dropped first when staffing is down.
During interviews it was also clear that turnover among staff and change was significant over the course of the year (between the baseline and follow-up visits). At follow-up facilities, managers were asked to update staffing information; however, the data collected were often incomplete. Therefore, they are not reported here.
Table 2. Average number of staff per unit at baseline (range), by training approach
| Traditional Training Approach | Modular Training Approach | Abbreviated Training Approach | |
|---|---|---|---|
| Prenatal Unit | |||
| Pediatric Unit | |||
| HIV Unit | |||
| Doctor | 4 (range: 1-7) | 2 (range: 0-5) | 3 |
| Nurse/midwife | 1 (range: 0-2) | 1 (range: 0-2) | 0 |
| Nursing assistant, aide, auxiliary | 1 (range: 0-2) | 1 (range: 1-2) | 0 |
| Community health agent | 0 (range: 0) | 0 (range: 0-1) | 0 |
| TOTAL | 6 (range: 2-11) | 4 (range: 1-7) | 3 |
| Doctor | 4 (range: 2-7) | 2 (range: 1-3) | 3 |
| Nurse/midwife | 3 (range: 0-5) | 1 (range: 0-2) | 5 |
| Nursing assistant, aide, auxiliary | 4 (range: 3-5) | 2 (range: 0-5) | 1 |
| Community health agent | 0 (range: 0) | 1 (range: 0-1) | 0 |
| TOTAL | 11 (range: 10-12) | 5 (range: 2-11) | 9 |
| Doctor | 2 (range: 2) | 1 (range: 0-2) | 2 |
| Nurse/midwife | 2 (range: 0-3) | 1 (range: 0-4) | 4 |
| Nursing assistant, aide, auxiliary | 5 (range: 0-10) | 1(range: 0-2) | 2 |
| Health educator/social worker/counselor | 0 (range: 0) | 1 (range: 1) | 0 |
| Pharmacist | 0 (range: 0) | 1 (range: 0-2) | 1 |
| Data manager | 0 (range: 0-1) | 0 (range: 0) | 0 |
| TOTAL | 9 (range: 2-15) | 5 (range: 3-7) | 9 |
Information on client load, which helps us understand the adequacy or inadequacy of staffing, was challenging to obtain. However, what was collected suggested significant variability between facilities (see Table 3). The MSPP’s online database, MESI, downloaded the average number of first prenatal visits each facility conducted for the period of October through December 2013. Data on pediatric clients’ attendance were not available, while data on HIV clients were collected from facility reports at baseline for the same time period. At baseline, the client-provider ratios varied significantly by facility and unit. The ratios were quite high in the prenatal and HIV units of the facility following the abbreviated training approach and in the HIV unit of the facilities following the traditional training approach. This information can help interpret the changes in provider practices as it suggests provider ability or time to integrate new nutrition services such as nutrition counseling.
Table 3. Average monthly client load and client-provider ratio per facility, based on facility reports from October–December 2013, by training approach
| Unit and Indicator | Traditional Training Approach | Modular Training Approach | Abbreviated Training Approach |
|---|---|---|---|
| Prenatal Unit | |||
| HIV Unit | |||
| Average monthly client load (average # of pregnant women seen in 1st prenatal visit) | 534 | 487 | 260 |
| Client-provider ratio | 29.6 | 37.5 | 86.7 |
| Average monthly client load (average # of clients seen in HIV unit) | 552 | 357 | 596 |
| Client-provider ratio | 50.2 | 23.8 | 66.2 |
Given the client load data, one would expect that Hôpital Notre Dame de Petit Goâve and Hôpital de Fort Liberté would have more staff. However, this was not the case. In fact, Hôpital Notre Dame de Petit Goâve reported having only five staff members at baseline – one of the smallest staff reported by facilities studied (data not show, but available upon request).
The Master Trainers
[I learned] A lot! I learned about nutritional in general, but I also learned about how to talk to mothers, how to consult and give recommendations. Before, I didn’t see myself talking to a patient about nutrition, but now I know how to do it, how to educate and convince a mother to eat a balanced diet.
—Trainer, Nurse, Emergency Unit
While all MTs were trained in the same fashion and during the same training, the effectiveness of any cascade trainings depended on the capacity of MTs to train HCWs (using the traditional or modular training approach) from their respective health facilities. A pre-training test was conducted before the TOT’s IYCF modules. After covering those TOT modules, the test was repeated. Trainees then were asked to complete another pre-test before covering the NACS modules. Given the overlap of some of the content, the pre-training test results related to the NACS modules should not be considered a true baseline of nutrition knowledge. This same test conducted before the NACS modules was repeated at the end of the training.
As indicated in the Table 4, the MTs working in both the traditional and modular training facilities learned key messages, though less so with regard to the NACS training modules. Fewer than half of the MTs passed the post-training test related to the NACS modules; however, the average test score was 75.0 percent among MTs from traditional training facilities and 77.5 percent among those from modular training facilities. This indicates some improvements over the pre-training test. The fact that improvements in test scores regarding the NACS modules were lower is not particularly surprising since this was the first time the training package was used.
Table 4. Pre- and post-training test scores among participants in the Training of Master Trainers, by training approach
| Average Scores | Traditional Training Approach(N=10) | Modular Training Approach(N=12) | Abbreviated Training Approach(N=3) | |||
|---|---|---|---|---|---|---|
| Pre-training | Post-training | Pre-training | Post-training | Pre-training | Post-training | |
| IYCF Modules | 50.4% | 89.0% | 49.4% | 91.1% | 44.6% | 93.8% |
| NACS Modules | 64.5% | 75.0% | 64.6% | 77.5% | 65.0% | 88.3% |
Master trainers remarked on how much they learned, how knowledgeable their trainers were, and how effective the training techniques were.
The methods and techniques they used during the training were really effective, and they had all the necessary materials. For example, we were able to practice on mannequins. There were mothers who came, and we taught them about the best positions to feed their babies. These practical components made our learning better.
—Trainer, Nurse, HIV Unit
However, MTs commented on the training being overloaded. Indeed, according to SPRING staff, the training could easily have been stretched out over 9–10 days instead of the 5.5 days in which the training had to be conducted due to budget and time constraints.
The Cascade Trainings
Based on reports from our staff members and interviews with trainers and trainees it became clear that the differences in how the trainings were ultimately rolled out in these seven facilities were fewer than had originally been envisioned when the concept for this research was designed based on two very distinct training approaches. It was anticipated, for example, that the more traditional training would use an out-of-facility venue. However, all trainings were conducted on-site in each of the health facilities.
We didn’t have enough time to absorb the information ... we couldn’t keep up with all the details. We tried to take notes, keep track of everything. But there’s only so much you write and digest when you’re going that fast.
—Trainer, Physician, Pediatric Unit
The only difficulty was that we had a lot of material to cover and not enough time … A person’s capacity to learn diminishes after a certain time, you know.
—Trainer, Nurse, Emergency
The time MTs took to roll out the training varied significantly. The content of the training (described above) that MTs were expected to roll out in their facilities was designed to take a minimum of 41.5 hours. Ideally more time should be spent to allow for practice and discussion. Those following the traditional training approach condensed the training into 5–10 consecutive work days for four to eight hours each day for a total of 40–60 hours of training; the facilities following a modular training approach conducted one – two sessions three times per week. Each session was between two and four hours each, and the entire training took 7–15 weeks to complete. The total number of hours spent was 32–94 hours. The MTs and facility managers of Hôpital Maternité Isaie Jeanty had initially planned to follow a traditional training approach; however, they ultimately only had two hours per day for the training, which was conducted over the course of two weeks (10 business days). For this reason, this facility is presented separately in the analysis that follows.
The specific approach and number of HCWs trained 1 in each facility was as follows:
Traditional training approach:
- Hôpital la Providence des Gonaives: one group of 26 HCWs, 10 consecutive work days for approximately six hours each day (≈60 hours), concluded in May 2014
- Hôpital Eliazar Germain: one group of 14 HCWs, 10 consecutive work days for four hours each day (≈40 hours), concluded in July 2014
- Hôpital Sainte Thérèse de Hinche: two groups of 12 and 17 HCWs, five consecutive work days for approximately eight hours each day, plus a refresher/catch-up training of 21 hours (≈61 hours), concluded in September 2014
Modular training approach:
- Centre Medico Social de Ouanaminthe: one group of 18 HCWs, three sessions per week for two hours each for approximately three months (≈72 hours), concluded in August 2014
- Hôpital de Fort Liberté: one group of 12 HCWs, two sessions per week for two hours each for eight weeks (≈32 hours), concluded in September 2014
- Hôpital Notre Dame de Petit Goâve: one group of 27 HCWs, two sessions per week for two to four hours each for approximately 15 weeks plus 3 four-hour refresher/catch-up training sessions (≈57 hours), concluded in August 2014
Abbreviated training approach:
- Hôpital Maternité Isaie Jeanty: two groups of 14 and nine HCWs, 10 consecutive work days for two hours each day, plus a one-week refresher/catch-up training of 12 hours (≈32 hours), concluded in June 2014
A total of 69 staff members were trained in facilities following the traditional training approach, 57 in facilities following the modular training approach, and 23 following the abbreviated training approach. The vast majority of the HCWs trained were nurses, midwives, or nurse/midwives, regardless of facility type.
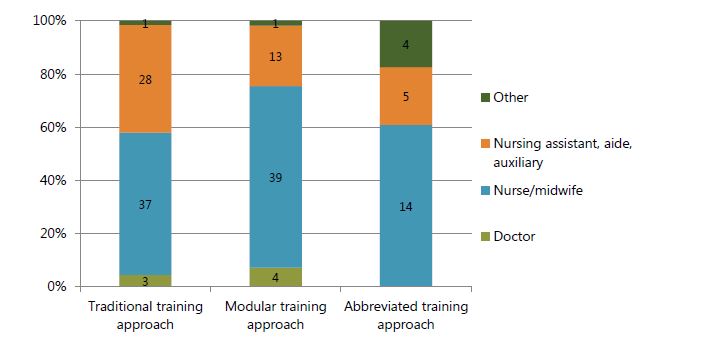
The majority of trainees from all facilities were nurses, midwives, and nursing assistants or auxiliaries (see Figure 1). Although MTs were instructed to prioritize staff responsible for providing assessment, counseling, and support services from the prenatal, pediatric, and HIV units, relatively few were from the HIV units of the targeted health facilities. The majority of the trainees were from the maternity, pediatric, or some other unit of the health facility (see Figure 2). Given the emphasis of the training on IYCF it is important to note that 24 percent of trainees from traditional training facilities were from the pediatric units, while 13 percent were from the pediatric unit in modular training facilities and only three percent were in the abbreviated training facility.
Figure 1. Number of people trained, by training approach and unit where the HCW worked at the start of the training
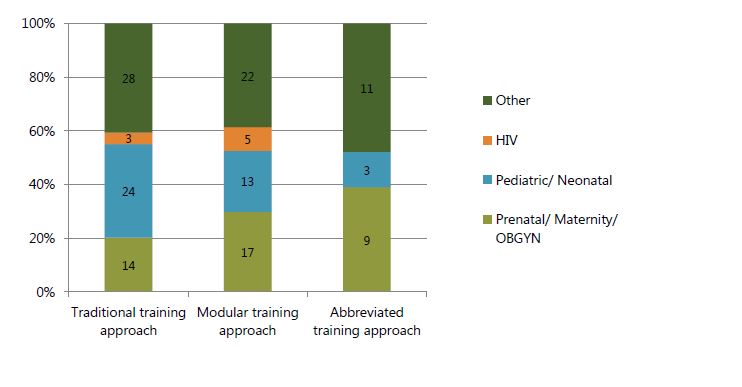
Figure 2. Number of people trained, by training approach and type of HCW
Another important finding is that modular training facilities lost more trainees to follow-up than facilities following the traditional training approach. This is most likely due to the extended period of time over which the training was conducted. As a result, even though the modular training approach started out with more trainees and was probably less burdensome for the trainees, the percent of trainees who completed the training in modular training facilities was fewer than in traditional training facilities (50 percent versus 77 percent) (see Table 5).
Table 5. Training outcomes, by training approach
| Traditional Training Approach | Modular Training Approach | Abbreviated Training Approach | |
|---|---|---|---|
| Number of trainees enrolled in the training | 74 | 80 | 25 |
| Number of trainees who completed the training 2 | 69 (93%) | 57 (71%) | 23 (92%) |
| Number of trainees who did not complete the training | 5 (7%) | 23 (29%) | 2 (8%) |
| Number of trainees who dropped out of the training | 4 | 19 | 2 |
| Number of trainees who left health facility without completing the training | 1 | 4 | 0 |
| Number of trainees who completed the training and are still on site | 57 (77%) | 40 (50%) | 23 (92%) |
Research Questions
How Receptive Have HCWs Been to Training in Facilities Following the Modular Training Approach Compared to Those Following a More Traditional Approach?
For any training to succeed it requires the active participation of trainees, as well as their receptivity to learn, which was determined by (a) perceived usefulness of the training; (b) receptivity of trainees to the MTs; (c) perceptions of the training among trainees; (d) perceived support from facility managers; and (e) incentives/motivation.
Oh, the whole training was great. The subject was interesting and very applicable to my work. I work in pediatrics, and we have a [malnutrition unit], so the knowledge I’ve acquired during this training has made a difference in the way I give counseling and talk to patients.
—Trainee, Nurse, Pediatric Unit
Perceived Usefulness of the Training
Interest in the topic can affect focus, attention, and effort exerted during trainings. During this research we explored trainees’ level of interest. Trainees from traditional facilities were more likely to report that the topic was very useful (93 percent) compared with those from facilities following the modular training approach (64 percent) and those following the abbreviated training (57 percent).
Although many respondents expressed interest in the topic during the interviews, trainers and trainees mentioned that participants should have been allowed to choose to participate instead of being picked or forced to attend.
A few participants also mentioned that the topic was not particularly relevant to their work since they worked in the emergency room or surgery unit. Some respondents commented on the selection of staff to be trained. While some felt that only permanent staff should have been trained (versus residents) others thought that only those who work in relevant units of the health facility should have been selected for the training.
Indeed, HCWs were sometimes selected out of convenience or because of their availability rather than for more strategic reasons such as relevance or interest. For example, many of those trained were residents who had more time available to participate, and a number of people trained currently work in units of the health facility where nutrition services are less of a priority or less feasible (e.g., emergency room, surgery, and pathology). Health care workers that should have received the training were often the most knowledgeable and skilled in a particular unit of the facility. Therefore, they were also the most needed in the facility. As a result, facility or unit managers opted not to send them to the training. This was observed in both facility types but more so in the traditional training facilities where colleagues and patients who struggled during the busy morning hours of consultation felt the HCWs’ absence more acutely.
To achieve good results, you have to have people who are well trained, and for this to happen, trainees have to participate voluntarily…they shouldn’t be forced. But if the training is taking place at work over many weeks, people can’t say that they’re absent, so they participate without really wanting to.
—Trainer, Nurse, Emergency Unit
The problem is that the large majority of the people who were trained were residents, so they’ve already stopped working at this facility. There are only a few of us participants who are left...
—Trainee, Physician, Emergency Unit
Let me tell you something. The nurses who work in pediatrics, for example, they can use what they’ve learned. They can take measurements and give counseling. But there are other nurses who were trained and never get to practice what they’ve learned because they work in other services that have nothing to do with nutrition. So all the effort we put training them has been wasted. For a training on nutrition, we need to focus on personnel in pediatrics and prenatal or on community health workers. But there’s no need to train someone who works in surgery. They don’t call me and tell me to partake in training about instruments used for surgery. It has no application for me. It doesn’t make sense… I think the training participants need to be picked carefully. It needs to be people in pediatrics, prenatal, HIV services.
—Trainer, Nurse, HIV Unit
Also, I think that the training should be targeted to personnel in different services. Instead of covering everything NACS/IYCF with all participants, for example, we should train the HIV staff for two days and cover only the parts of the training that apply to them; then do the same thing with the prenatal personnel for two days; and so on. That way, we’ll only be covering the information that people will use in their work, and coordinating schedules will be easier because we’ll have to worry about two days instead of a whole week.
—Trainer, Physician, Malnutrition Unit
Receptivity of Trainees to the Master Trainers
As mentioned before, all MTs were trained during the same TOT and all were staff from the targeted health facilities. Master trainers and trainees commented on the advantages of training by and for health facility staff. Trainees felt comfortable being trained by MTs from their own facilities because they already knew them. They also appreciated that MTs from their own facility would remain in the facility to clarify material learned. Similarly, trainees said that the MTs were familiar with the realities of the health facilities.
However, several trainees from both types of facilities also mentioned that being trained by colleagues is not the same as being trained by a “true professional.” Additionally, one trainee mentioned that tension can arise when trainers are colleagues who may be younger or are friends because they may not be taken as seriously as an external trainer. At least one MT echoed this sentiment.
It was very good. We asked many questions. We didn’t feel uncomfortable to ask questions because it was our own colleague teaching us. And she was well trained. We were comfortable. It’s hard for us to feel comfortable and ask questions when it’s someone we don’t know. But if it’s one of us teaching, we feel comfortable to voice our questions and ask her to clarify if we don’t understand.
—Trainee, Nurse, Emergency Unit
It was good. We had a lot of fun because we already knew each other. It was better... We laughed and we learned better because we were already comfortable with them.... I was comfortable training my colleagues because I knew most of them. And they knew me, so they felt free to ask me questions. Some people are timid, you see, and they refrain from asking questions to someone they don’t know because they don’t know how that trainer will react to their questions. But we all knew each other, so I felt comfortable with them and they felt comfortable with me.
—Trainee, Nurse, PMTCT Unit
They are here, even after the training. So we can call on them at any time for help or clarification.
—Trainee, Nurse, Pediatric Unit
We could talk specifically about the realities of working at this institution with them. We couldn’t have discussed in such a way with an outsider because s/he wouldn’t understand.
—Trainee, Nurse, Pediatric Unit
…these trainers work here with us, so they know the needs of the community…they know about the taboos that lead to malnutrition in children.
—Trainee, Physician, Emergency Unit
Perceptions of the Training Among Trainees
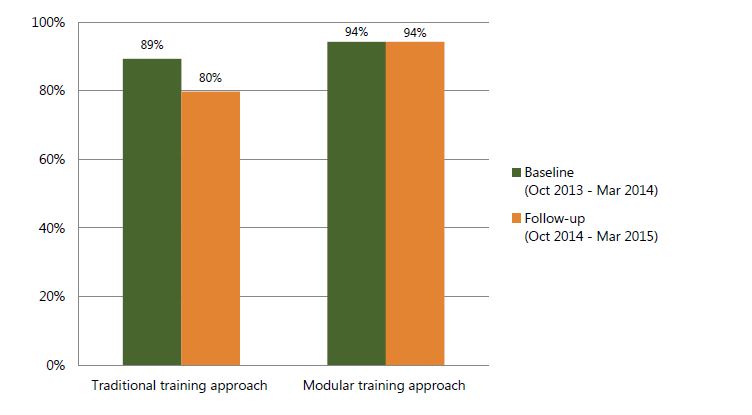
Overall, trainees from facilities following the modular training approach were more satisfied with the training compared with those from facilities following the traditional training approach (85 percent versus 73 percent) (see Figure 3). In particular, they were more satisfied with the organization, materials/ handouts, and the length of the training (see Annex Table 1).
Figure 3. Percent of trainees satisfied with the training, by training approach
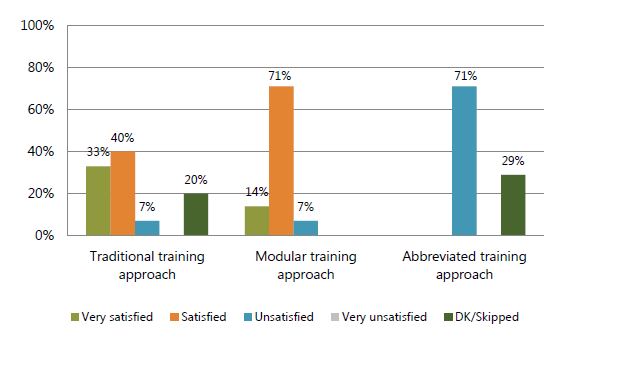
In the case of the materials/handouts, all trainees should have received the same materials. However, those participating in the modular trainings likely had more opportunity to review and use the materials since, on average, facilities following the modular training took more time to complete the training. We also explored whether trainees in facilities where more time was spent on the training, regardless of the approach, were more or less satisfied. No trends were observed.
Perceived Support From Facility Managers
The feedback we received from several MTs was that the facility managers were not supportive. Master trainers commented on the lack of adequate space for the training, stand for flip charts, a projector, and energy source to run the projector. Project staff found that MTs were often expected to conduct the trainings while maintaining their usual workload in the facility. In addition, according to SPRING staff and based on reports from MTs, facility managers did little to motivate the trainees to be on time and be fully present and involved in each training session (regardless of training approach). Furthermore, with the traditional training approach, SPRING and MTs were able to manage expectations better, explaining to facility managers that we need staff (including the MTs) for a precise number of hours and a precise time period; in contrast, with the modular approach, MTs needed to gain approval for every session. As a result, managers, MTs, and trainees from facilities following the modular approach were often frustrated after several weeks of the training. For this reason, facility manager support was even more critical in facilities following the modular training approach.
Incentives/Motivation
Other than a certificate from the training, we are not aware of other incentives that facility managers provided to motivate trainees to participate in the training. When interviewed, many trainees expressed disappointment that they still had not received their certificates—that they did not have anything to show that they had participated in this training. Unfortunately, this is a product of the training approach selected. Trainees were not eligible to receive a certificate until MTs had submitted documentation of participation and passing scores on the post-training test. As mentioned before, many facilities struggled with attendance and, therefore, post-training test scores.
We didn’t receive the certificates. We worked really hard, so it’s disappointing to not have something that proves our participation and completion of that training. We’ve tried to ask the trainers, but they don’t have any information.
—Trainee, Volunteer community health worker, HIV Unit
It would be good if the trainees here received their certificates. They’ve been waiting eagerly and are really discouraged that they still haven’t received their certificates.
—Trainer, Nurse/Surgery unit manager, Surgery Unit
We’re a little disappointed because we still haven’t received the certificates. We don’t have anything to show that we’ve taken this training.
—Trainee, Nurse, Pediatric Unit
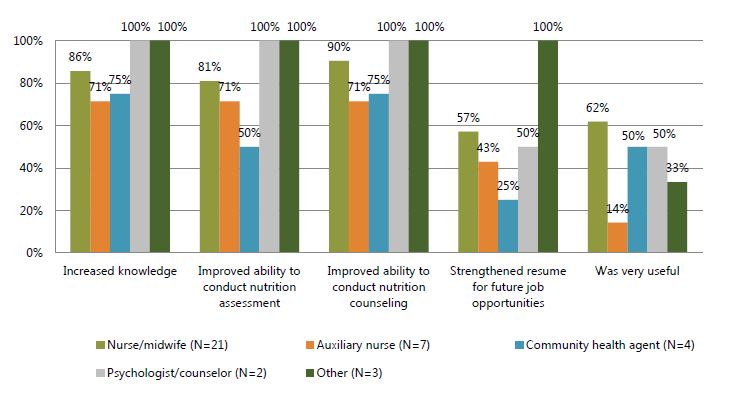
When surveyed, trainees from facilities following the traditional training approach were more likely than those from facilities following the modular training approach to confirm that the training increased their knowledge, improved their ability to conduct nutrition assessment and counseling, and strengthened their resumes for future job opportunities (see Figures 4 and 5).
Figure 4. Percent of trainees who reported various benefits from the training, by training approach
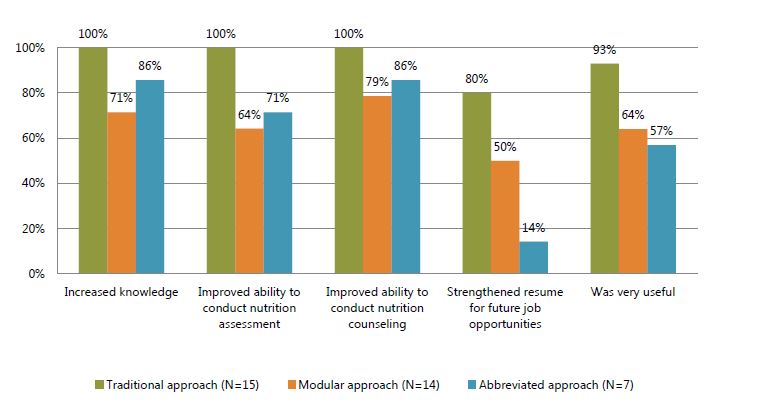
Figure 5. Percent of trainees who reported various benefits from the training, by type of health care worker
To What Extent Has the ELC Been Followed By MTs in Facilities Following the Modular Training Approach Compared With Those Following the More Traditional Training Approach?
Evidence suggests that a key determinant of the success of any training, particularly for adults, is the extent to which the ELC is followed. The ELC brings together what is known about adult learning, building on the principles that Erik Erikson, Malcolm Knowles, Lyra Srinavasan, Paolo Freire and many others outlined. By using it deliberately and consistently, MTs can help people develop the skills, knowledge, and attitudes that will lead to continuous learning and lifelong change. Under this objective, therefore, we explored questions related to that cycle: (a) whether the training built on what trainees already knew; (b) whether trainees had the time and space to reflect on the new information shared during the training; and (c) whether trainees had the opportunity to practice new knowledge. Each is explored in the section below.
The problem was time and availability... we had two weeks of training, which wasn’t sufficient since we had only a few hours per day. And we were being interrupted on top of that. We needed more time to cover the material in detail, to analyze, to revise. It wasn’t enough time to digest the information. We covered all the modules, but we did it in such a rush.
—Trainee, Nurse, Prenatal Unit
The topics covered were very overwhelming. It was a lot of information and not enough time to talk, exchange ideas and digest the information. Personally, I had to come and go during the training because I’d sometimes have work to do in between.
—Trainee, Nurse, Vaccinations
Building On What Is Known
We were interested in finding out if MTs found out what participants already knew and built on that knowledge during the training. This ensures that the training addresses perceived problems or gaps in knowledge. It also saves time because it avoids MTs repeating content that the training participants already knew (and might find boring or irrelevant) or backtracking to introduce information they assumed participants already knew. Finally, by using participants’ experiences as a point of departure for introducing new information, MTs built a trusting and respectful atmosphere that is necessary for learning.
Table 6. Trainees’ perceptions of qualifications of Master Trainers, by training approach
| Traditional Training Approach (N=15) | Modular Training Approach (N=14) | Abbreviated Training Approach (N=7) | |
|---|---|---|---|
| Asking for trainee’s input based on his or her past experiences and knowledge | |||
| Very qualified | 67% | 36% | 0% |
| Qualified | 13% | 43% | 43% |
| Unqualified | 7% | 7% | 0% |
| Very unqualified | 0% | 0% | 0% |
| DK/Skipped | 27% | 14% | 57% |
In the spirit of qualitative research, we did not ask questions directly about this topic, hoping it would come up naturally without leading questions. Unfortunately, it did not. Therefore, we are left wondering if it was because MTs did not build on what trainees knew (because it is not their style or because they felt that trainees did not have much knowledge at the start to build on) or simply because it did not occur to trainees to mention this. What we do know is that about 80 percent of trainees in facilities following the traditional and modular approach felt that trainers were qualified or very qualified at asking for input from trainees’ past experiences or knowledge (see Table 6). In the facility following the abbreviated training approach, where MTs had significantly less time for the training, trainees reported lower confidence in their trainers’ ability to ask for input.
Time and Space to Reflect
Another aspect of the ELC has to do with having the time, space, and structure to reflect on and think critically about what trainees had been learning during the training. This is done to figure out if the training was important to them and to consider how they would use what they had learned. Likewise, it is important for learners (trainees) to reflect on actions in the “real world.” Trainees from all facility types reported that MTs provided opportunities for trainees to give feedback and ask questions (see Table 7).
Table 7. Trainees’ Perceptions of qualifications of Master Trainers, by training approach
| Traditional Training Approach (N=15) | Modular Training Approach (N=14) | Abbreviated Training Approach (N=7) | |
|---|---|---|---|
| Providing opportunities for trainee to give feedback or ask questions | |||
| Very qualified | 67% | 57% | 29% |
| Qualified | 27% | 29% | 71% |
| Unqualified | 0% | 0% | 0% |
| Very unqualified | 0% | 0% | 0% |
| DK/Skipped | 4% | 14% | 0% |
[The [modular training approach] was good because] the hospital can continue to provide services because the training was only a few days a week for about two hours. The daily functions of the hospital weren’t disturbed.
—Trainer, Nurse-midwife, Maternity Unit
During in-depth interviews in traditional facilities, several trainees mentioned that the training was overloaded and that they did have adequate time to focus and learn. In Hôpital Maternité Isaie Jeanty where an abbreviated training approach was followed, the training was conducted in the least amount of time. As a result, eight of the nine interviewees mentioned that the training felt overloaded.
Participants also commented that they were not able to concentrate because they were on-site and were frequently interrupted and called to work. Participants from both types of facilities made this comment, but it was more frequent among trainees participating in the full-day trainings of the traditional approach.
We’re all professionals, and we were doing the training right here, on site. So we still had obligations to fulfill. We couldn’t take too long with the training... It’s the disadvantage of an on-site training. If we could go somewhere where we could really focus, it would have been great. But here, all of us had obligations, and this affected the efficacy of our message. An on-site training has many constraints. But if training is offsite, the ambience is neutral and allows for concentration.
—Trainer, Physician, Pediatric Unit
What I didn’t like was the location. We were trained right here at work, so we were called on when needed. We were forced to leave the training to attend to one thing or another. We couldn’t give our full concentration because we were being interrupted so regularly.
—Trainee, Volunteer community health worker agent, HIV Unit
Trainees from modular training facilities were more likely to mention that that they had more time to digest the information since the training was only a few hours each time and since they were able to continue working for part of the day.
Every session takes about two hours, and it’s only twice a week. So, I learn a few things during these sessions and then have time to digest the information. If all training is done in one week, it’d be hard for me to keep everything in my head. Especially after work, it’d be impossible. I can’t do more than two hours of training after work!
—Trainee, Nurse-midwife, Maternity and Prenatal Units
With the traditional approach, the whole training is packed within a week or two, and there’s limited time to digest the information. [...] In the end, I prefer the [modular training approach] because the information we learned is too much for one week!
—Trainee, Physician, Emergency Unit
Opportunities to Practice New Knowledge
Next, SPRING explored the extent to which participants were given opportunities to put into practice the knowledge and skills taught during and after the training. Doing so helps learners to master new practices and build confidence while also helping MTs and the learners see the progress being made. Trainees from the facilities following the traditional training approach (80 percent) and modular training approach (86 percent) were more likely to report having had an opportunity to provide nutrition counseling since the training compared with the facility that followed the abbreviated training approach (71 percent) (Table 8).
Table 8. Trainees’ Perceptions of qualifications of Master Trainers, by training approach
| Traditional Training Approach (N=15) | Modular Training Approach (N=14) | Abbreviated Training Approach (N=7) | |
|---|---|---|---|
| Providing opportunities to practice the new knowledge or skills taught | |||
| Very qualified | 73% | 29% | 14% |
| Qualified | 13% | 57% | 43% |
| Unqualified | 0% | 0% | 0% |
| Very unqualified | 0% | 0% | 0% |
| DK/Skipped | 22% | 14% | 43% |
Consistent with these findings, when interviewed, trainees from facilities following the modular training approach were more likely to report having an opportunity to practice what they had learned. However, several trainees from both types of facilities expressed disappointment that they were not given enough time to practice counseling skills during the training. Additionally, a higher percentage of trainees from the facility following the abbreviated training approach (43 percent) reported having experienced challenges with providing nutrition counseling compared with those from facilities following the traditional training approach (20 percent) and the modular training approach (7 percent).
[The modular training approach is] better because it allows participants to really digest the information because they can practice on patients in between sessions, but it’s really hard to coordinate availability and to guarantee concentration.
—Trainer, Nurses' manager, Maternity Unit
Well, with the traditional approach, people are available and are able to concentrate because there’s a block of time—a week or two weeks—that have been specifically set aside for the training. But it’s also really hard to internalize all the information… With the [modular training approach], we take longer and go slower, which gives participants time to digest the information and gives them time to practice at work in between sessions.
—Trainer, Nurses’ manager, Maternity Unit
The sessions were more spread out with the OJT [on-the-job training], which gave us a chance to practice in between. But I’d prefer to get trained in the traditional way and then practice after I come back to work.
—Trainee, Nurse, Maternity Unit
I learned about the position for breastfeeding a baby and about how we should welcome and give counseling to patients. We practiced this with each other.
—Trainee, Nurse’s aide, Prenatal Unit
We faced another difficulty when we asked participants to contribute some items so we could all practice preparing food as part of the training. There were no funds, and participants weren’t able to contribute, so we couldn’t practice that part. We even had to practice counseling amongst ourselves because patients weren’t coming to the hospital due to the protests. Practicing with patients would have been much better.
—Trainer, Nurses’ manager, Maternity Unit
I learned a lot, but all of this was in theory because we didn’t really have time to practice on mannequins and to study the posters, and we didn’t have a chance to test our counseling skills with pregnant women... We did [get to practice], but there wasn’t enough time for us to really feel comfortable with the material. We really needed more time, and the environment didn’t help.
—Trainee, Nurse, Biopsy
What Are the Costs of Rolling Out the Training Following the Modular Training Approach Compared With the More Traditional Approach?
The cost of different training approaches is an important consideration as governments and programs plan to scale up. Governments, programs, facilities, individual trainees, or health facility clients bear the costs, including the financial and opportunity costs.
For this research, we opted to focus on estimated average financial costs to avoid conflating context-specific differences in costs with differences in costs due to the training approach (see Table 9). For this exercise, we assumed 25 trainees would be in attendance. We also assumed that the modular training approach would be rolled out in 20 sessions and that the traditional training would be five full days. Per diem for the offsite training was estimated for six days for all trainees, assuming one day for travel.
Table 9. Estimated costs of training Cascade, by approach and location (in US Dollars), by training approach
| Item | Traditional Training Approach (on-site) | Traditional Training Approach (off-site) | Modular Training Approach (on-site) |
|---|---|---|---|
| Conference room | $0 | $500 | $0 |
| Transportation-participants | $0 | $5,500 | $0 |
| Supplies | $250 | $250 | $250 |
| Per Diem | $0 | $14,489 | $0 |
| Food | $1,847 | $0 | $1,455 |
| Honorarium for trainers | $364 | $364 | $909 |
| Phone cards | $0 | $114 | $0 |
| Total | $2,097 | $20,739 | $1,705 |
None of the people interviewed (including facility and unit managers, as well as trainers and trainees) mentioned costs of the trainings borne by patients. However, they did comment on being distracted by participants frequently leaving the training to attend to patients.
What Knowledge Has Been Gained By HCWs Trained in Facilities Following the Modular Training Approach Compared With Those Trained Following the More Traditional Training Approach?
Even if trainings are well received by trainees, they can only be considered successful if they improve knowledge and the quality of services provided. Trainees were assessed before and after trainings. By the conclusion of the training modules, approximately 90 percent of trainees had passed the post-training test by scoring at least 70 percent (see Table 10).
Table 10. Post-training test results among participants in the cascade trainings*, by training approach (%)
| Traditional Training Approach (N=69) | Modular Training Approach (N=57) | Abbreviated Training Approach (N=14) | |
|---|---|---|---|
| Percentage of trainees who took the post-training test and scored ≥ 70 percent | 84%* | 93% | 93% |
* In Hôpital Sainte Thérèse de Hinche, a traditional training facility, and Hôpital Maternité Isaie Jeanty, where the abbreviated training approach was followed, very few or none of the trainees passed the post-training test at first. As a result, the trainers conducted several two – three-hour catch-up sessions (~12 additional hours of training), focusing on areas of weakness among trainees and answering questions. Staff members from SPRING also conducted one supervisory visit. As a result, post-training test scores were raised to passing.
During interviews, trainees mentioned learning about the following:
- Nutrition assessment/monitoring (mid-upper arm circumference [MUAC], weight, height, etc.)
- How to recognize a malnourished client
- What to do or how to interpret anthropometric measures
- Nutrition counseling. listening and talking to patients
- Importance of the 1,000 days
- Importance of breastfeeding
- Breastfeeding positions
- “Tactics to make the milk come out”
- HIV and breastfeeding
- Benefits of breastfeeding to the family and community
- Food mothers should eat
- Complementary foods
- Which foods to feed children depending on age
- How to have a balanced diet
Have Nutrition Services Changed As a Result of the Trainings? How Do Changes Vary Between Facilities Following the Modular Training Approach and Those Following the More Traditional Training Approach?
By reviewing registers and electronic medical records, as well as observing client-provider interactions, we were able to determine the degree to which services changed in the two types of facilities. Through in-depth interviews, the project explored trainees’ experiences putting knowledge into practice. We also explored the factors that constrained, enabled, encouraged, or supported adoption of new practices.
Trainees from facilities where the traditional and modular training approaches to rolling out the training were used found that the training had enabled them to provide better nutrition service. Trainees said the training has allowed them to share better, fuller information with their patients and has taught them how to talk to patients. Changes/improvements in counseling (especially about breastfeeding and balanced diet) were mentioned the most. Respondents also talked about taking anthropometric measurements correctly and more frequently and knowing how to interpret the results. They also talked about recognizing malnourished cases better/being more aware about malnutrition. Many trainees equated these changes to improved quality of services in their facilities.
It’s the same personnel that does everything. When you have an employee who comes to work and has to see 80 children per day…and who’s asked to measure the weight of each, to everything else she has to do…it’s impossible. It’s certainly not something that is prioritized, do you understand? Nutrition diminishes as a priority. It’s not easy. Even with the application of NACS—sure it’d be great if you had a designated doctor, say, in pediatrics, where you could send children who appear malnourished. But that’s not the case…doing NACS in an institution like this one is not easy! How can a doctor who sees 50, 30, 40 children a day do NACS….How does he find the time to talk to each mother about what she’s feeding to her child, what her economic status is, what she can afford? It’s really not easy in an institution like this that receives so many children and has the same doctor who’s doing everything. But if there was a doctor whose responsibility centers around promoting NACS, then he’d have maybe 15 patients to see in a day, and he’d have the time to give counseling to patients about nutrition. But it’s not easy to listen to 30, 40, 50 parents every day, in addition to everything else the doctor has to do…no! Really, NACS is definitely not a priority right now. The priority is to treat children who come to the hospital with medical problems…and maybe we’ll say gloss over nutrition here and there, but it’s not a true consultation like what we learned in NACS, you understand? It’s not easy.
—Trainer, Nurse, Emergency Unit
Nutrition Assessment
Respondents complained about their inability to put knowledge into practice because of a lack of equipment or materials. Indeed, according to unit managers, health facility units visited were not adequately equipped for nutrition assessment (see Table 11). To properly assess the nutritional status of their clients, prenatal units should have at least one MUAC tape for adults; pediatric units should have at least one functioning scale for children, height board, and MUAC tape for children; and HIV units should have all of the above since this unit can see patients, young and old, who are pregnant and not pregnant.
Table 11. Equipment for nutritional assessments at follow-up, by training approach
| Percentage of Facilities Adequately Equipped for Nutrition Assessment | Traditional Training Approach | Modular Training Approach | Abbreviated Training Approach |
|---|---|---|---|
| Prenatal unit | (N=2) | (N=3) | -- |
| Pediatric unit | (N=3) | (N=2) | -- |
| HIV unit | (N=3) | (N=3) | (N=1) |
| Adequately equipped to assess nutritional status of pregnant women | 100% | 100% | -- |
| At least one MUAC tape for adults | 100% | 100% | -- |
| Adequately equipped to assess nutritional status of children | 100% | 50% | -- |
| At least one length board (for infants) owned | 100% | 50% | -- |
| At least one infant/pediatric scale owned and functional | 100% | 100% | -- |
| At least one MUAC tape for children | 100% | 100% | -- |
| Adequately equipped to assess nutritional status of all PLHIV clients | 25% | 0% | No |
| At least one length board for infants owned | 33% | 0% | No |
| At least one infant/pediatric scale owned and functional | 66% | 66% | -- |
| At least one MUAC tape for children | 33% | 66% | Yes |
| At least one height board for adults owned | 66% | 66% | -- |
| At least one adult scale owned and functional | 100% | 66% | -- |
| At least one MUAC tape for adults | 100%* | 100% | Yes |
*One of the three HIV units in traditional training facilities reported that the MUAC tape for adults was shared with another unit.
Although not always used, as indicated by the observations, all the prenatal units visited had at least one MUAC tape for adults. All the pediatric units in traditional training facilities were adequately equipped for assessing the nutritional status of children; however, of the two facilities following the modular training approach, only one was. The pediatric unit in Centre Medico Social de Ouanaminthe did not have a functioning length board for infants at the time of the follow-up visit (data not shown, but available upon request).
Finally, only one of the six HIV units was adequately equipped to measure the nutritional status of HIV-positive pregnant women, children, and adults. This may suggest that our expectations for the HIV units may not be in accordance with the expectations of facility managers or HIV units. However, assuming they do attend to PLHIV of all ages, our expectations were in line with the protocols for assessing nutritional status of such clients.
Nonetheless, many trainers and trainees mentioned improvements in nutritional assessment (measurement, classification, and use of findings). Nutritional assessment was defined as clients under 18 years with age, sex, height, and weight recorded to calculate weight-for-height z-scores (WHZ) or body mass index (BMI) for age z-scores; pregnant clients with MUAC recorded; and adults 18+ years old with age, height, and weight recorded to calculate BMI.
Our review of data from facility registers was inconclusive. Registers in most prenatal and pediatric units did not have enough up-to-date data to determine if nutrition services (assessment, classification, counseling, or referral) were provided. At follow-up, many facilities were no longer maintaining or completing the columns related to nutritional status in the registers. Health facility staff complained of the heavy burden of reporting requirements.
MSPP now asks us to complete reports on nutrition, but we’re a public institution, and we have many difficulties in trying to do this…technical problems, administrative problems, and others. MSPP asks a lot of us but doesn’t provide us with sufficient personnel. How can we fill out nutrition reports if there aren’t enough nurses to do the regular work? There’s no one person who’s responsible for nutrition; there’s no one designated to give nutritional counseling, no one person where we could send patients to get nutritional counseling. We try to talk to patients about nutrition here and there, but there’s no structure in place for us to do this systematically.
—Trainer, Nurse, Emergency Unit
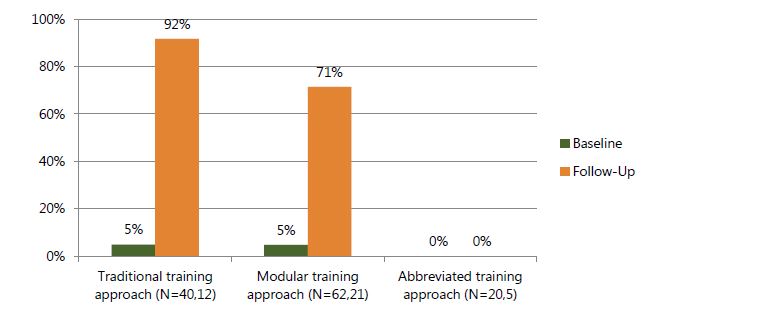
However, observations of client-provider interactions provided some insight into the nutrition assessment practices of providers (see Figures 6a, b, and c). Improvements were observed in all units. Given the small sample size of observations in the facility following the abbreviated training approach, findings were less conclusive.
In the prenatal units (Figure 6a), the percentage of pregnant women who were nutritionally assessed (MUAC measured/reviewed) was dramatic in both the traditional and modular facility types, but at follow-up it was greater in traditional facilities (92 percent versus 71 percent).
Figure 6a. Percentage of prenatal clients nutritionally assessed according to guidelines, based on observation, by time point and training approach
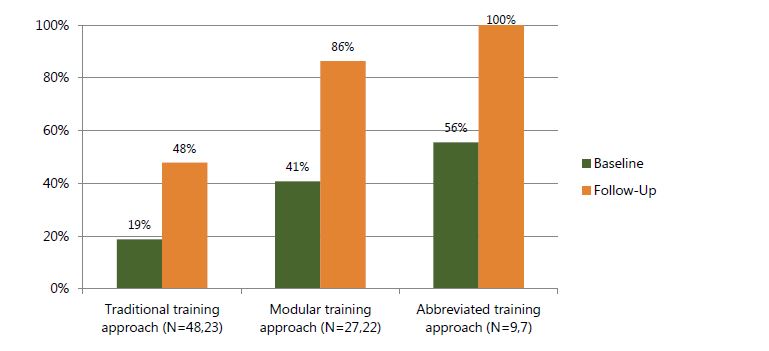
In pediatric units (Figure 6b), improvements were observed in both the traditional and modular training facilities, but at follow-up, the percentage of children who were nutritionally assessed according to guidelines was higher in modular training facilities (48 percent versus 86 percent). This is primarily due to height not being measured or reviewed.
Figure 6b. Percentage of pediatric clients nutritionally assessed according to guidelines, based on observation, by time point and training approach
Finally, in the HIV units of both the traditional and modular training facilities (Figure 6c), we observed improvements in the assessment of nutritional status. However, these figures mask the variations in each facility. We observed improvements in two traditional training facilities: Hôpital Sainte Thérèse de Hinche and Hôpital la Providence des Gonaives; however, in Hôpital Eliazar Germain, the percentage of clients nutritionally assessed according to guidelines declined from 100 percent at baseline to 86 percent at follow-up primarily due to a reduction in clients whose height was measured. In two of the three facilities following the modular training approach, 100 percent of the clients were assessed according to guidelines at baseline and follow-up.
Figure 6c. Percentage of HIV clients nutritionally assessed according to guidelines, based on observation, by time point and training approach
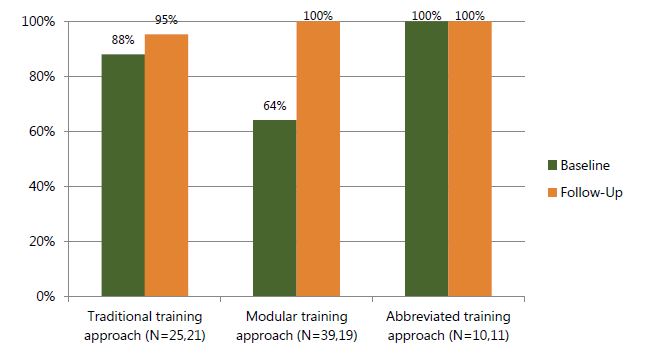
In the facilities following the modular approach, the percentage increased from 64 percent to 100 percent. The low percentage at baseline was because only 22 percent of the observation was height measured in Hôpital Notre Dame de Petit Goâve.
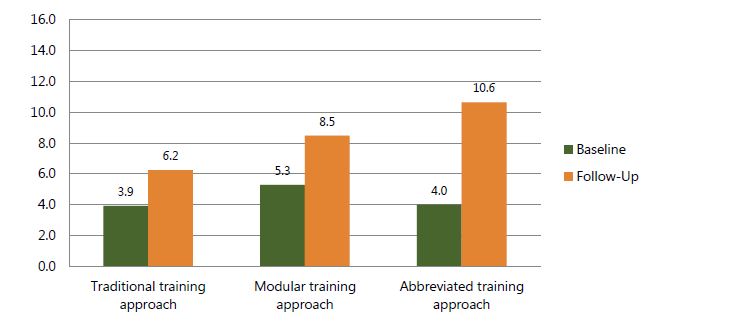
Also, in HIV units where the iSanté EMR system is used, we analyzed data from two of the traditional training facilities (Hôpital Eliazar Germain and Hôpital la Providence des Gonaives) and all three modular training facilities (see Figure 7). We calculated the percentage of new clients whose nutritional status was assessed according to guidelines during the six-month period before rolling out the training (October 2013– March 2014) and again during the six-month period after rolling out the training (October 2014–March 2015).
In the two traditional facilities included in this analysis, the percentage of clients nutritionally assessed according to guidelines declined from 89 percent during the six months before the rollout of the training to 80 percent during the last time period, which was approximately 3–9 months after the training. Consistent with observations, a dramatic decline was calculated in Hôpital Eliazar Germain—from 92 percent to 71 percent after the training. This is because neither age nor pregnancy status was recorded in iSanté during this time period. Without this, we were unable to determine the proper measure of nutritional status: WHZ, BMI-for-age, BMI, or MUAC. In the three modular training facilities, the percentage remained constant at 94 percent. Furthermore, Hôpital Sainte Thérèse de Hinche, which was not included in this analysis, was one of the facilities that demonstrated the greatest improvements during observations.
Figure 7. Percent of PLHIV nutritionally assessed according to guidelines, based on the iSanté EMR system six months before rolling out the training (October 2013–March 2014) and six months after (October 2014–March 2015) 3 , by time point and training approach
Nutrition Counseling
Respondents (trainers and trainees) commented on improvements in nutrition counseling after the training. Many highlighted improvements in breastfeeding support.
The mean numbers of counseling skills observed are presented in Figures 8a, 8b, and 8c. These reveal that the mean number of counseling skills observed increased in the pediatric and HIV units from baseline to follow-up in all facility types. However, counseling skills observed in the prenatal units remained roughly constant between baseline and follow-up. Some of the most dramatic improvements were observed in HIV units, particularly in the facility following the abbreviated training. In addition, a number of the specific nutrition counseling skills the SPRING/Haiti prioritized saw improvements, although the figures were still quite low (see Annex Table 3).
Figure 8a. Mean number of nutrition counseling skills observed in prenatal units, by time point and training approach
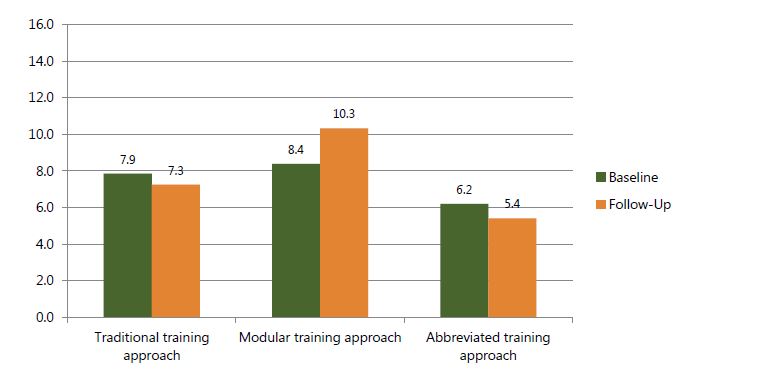
Figure 8b. Mean number of nutrition counseling skills observed in pediatric units, by time point and training approach
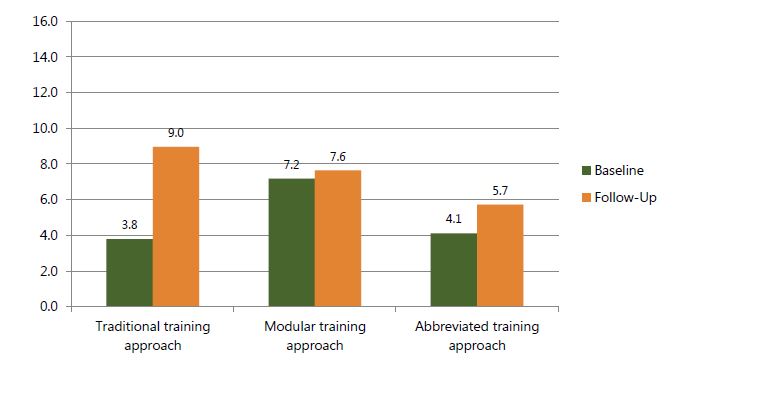
Figure 8c. Mean number of nutrition counseling skills observed in HIV units, by time point and training approach
However, during interviews, respondents noted challenges as well. With limited time and staff, there is rarely enough time to dedicate to the proper provision of nutrition counseling.
[In the prenatal unit] there isn’t enough time to do nutritional counseling with all our patients, but if someone looks malnourished or is anemic or gains too much weight during pregnancy, we talk to them about nutrition... like I said, nothing much has changed... We are always overloaded with patients. We don’t have enough personnel, so there’s no time to give nutrition counseling to every patient. […] But maybe, if we had videos to play in the waiting rooms, so that patients can learn something about nutrition while they wait, even if the nurses and doctors don’t have time to talk to them about it, it would be good.
—Trainer, Nurse-midwife, Maternity Unit
Nutrition Support
Unfortunately, many respondents from both facility types equated the lack of supplies to not having/offering nutrition services. Indeed, none of the facilities had iron–folic acid (IFA) supplements, dry rations, or ready-to-use therapeutic food in stock at the time of the follow-up visit. Only two modular training facilities had vitamin A in stock, and only one traditional training facility had multivitamins and deworming medication.
Respondents felt that they were unable to put knowledge into practice because of supply shortage/ stockouts. When observed, providers did not prescribe nutrition products since, in most cases, supplies were not available. Nor did they refer prenatal or pediatric clients to support services (see Table 12). Only in the HIV units did providers refer clients to support services (community worker or social support)—38 percent of observations in traditional training facilities and 74 percent of observations in modular training facilities.
We don’t have anything to give to our patients, except for counseling. How are we supposed to review the quality of that? There are no nutrition services for us to evaluate!
—Trainer, Nurse-midwife, Maternity Unit
Table 12. Nutrition support provided, based on observation, by time point and training approach (improvements shaded in green, declines shaded in gold)
| Percentage of client-provider interactions observed during which time the provider… | Traditional Training Approach | Modular Training Approach | Abbreviated Training Approach | |||
|---|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | Baseline | Follow-up | |
| Prenatal Unit | (N=40) | (N=12) | (N=62) | (N=21) | (N=20) | (N=5) |
| Pediatric Unit | (N=48) | (N=23) | (N=27) | (N=22) | (N=9) | (N=7) |
| HIV Unit | (N=25) | (N=21) | (N=39) | (N=19) | (N=10) | (N=11) |
| Referred client to support services (family planning, community worker, or social support) | 3% | 0% | 5% | 10% | 0% | 0% |
| Referred client to support services (community worker or social support) | 0% | 13% | 0% | 9% | 0% | 0% |
| Referred client to support services (community worker or social support) | 12% | 38% | 3% | 74% | 0% | 27% |
The large majority of interviewees responded that they had not received any formal follow-up after the training aside from the one we provided. However, trainees did note that trainers followed up with them during informal or impromptu discussions, inquiring about experiences using the knowledge acquired; a few respondents mentioned informally discussing the quality of nutrition services provided. Others commented that it was not possible to discuss quality of nutrition services until nutrition services (i.e., food) are provided. This was true in traditional and modular training facilities.
There’s nothing structured or formal, but we try to discuss, within our units, about what we could improve in the future.
—Trainer, Nurse, Maternity Unit
One of the trainers checks the quality of the services given by nurses and student nurses. [...] she goes around and makes sure that we’re all talking about breastfeeding to our patients.
—Trainee, Nurse-midwife, Maternity and Prenatal Units
Yes, we discuss about our services... No [we don't talk specifically about nutrition], we just talk about health services in general. We don’t focus on nutrition. We need to first provide nutritional services and materials before we can evaluate the quality of such services.
—Trainee, Nurse’s aide, Prenatal Unit
Limitations and Challenges
This study had several important limitations resulting from the fact that this was implementation research exploring SPRING/Haiti’s existing plans for implementation. The plans were designed in collaboration with the USAID mission in Haiti and the MSPP. It was not an intervention designed specifically to answer the research questions. First, data were not collected in comparable control health facilities. Therefore, we were unable to make assertions about what might have happened in the absence of training and other support we provided. Any changes in nutritional services cannot be fully attributable to the project.
Components of Human Performance: What Is Required for a Worker to Do the Job
Knowledge, skills, and capacity
- Does the individual know the task and can he or she perform it competently in an effective and efficient manner?
- Does the individual have the physical, mental, and emotional capacity to perform the tasks?
Attitudes and motives (internal)
- Does the individual see value in the ability to perform the task?
Data and information
- Does the individual know what he or she is expected to do (job description, scope of work, contract, etc.)?
- Does the individual have access to the information needed to do the job (job aids, procedure manuals, data for processing, etc.)?
- Does the individual receive feedback on his or her performance of the task (feedback reports, supervision)?
Tools and resources
- Does the individual have all the materials and tools needed to perform the task?
Setting
- Does the individual perform the task in a physical and social environment that allows him or her to perform the task adequately?
Incentives (external)
- Does the individual receive adequate compensation and recognition for performing the task?
Second, the lack of equipment and supplies, as well as the physical space for counseling, was a major barrier to putting knowledge into practice. Similarly, the fact that many facilities rely heavily on social service residents resulted in attrition and turnover of trained staff. These factors, which were not within the control of SPRING or this research activity, reduced the chances of providers to put knowledge into practice or of nutrition services improving in the targeted facilities.
Third, while we recommended two distinct approaches to rolling out the training, it was the trainers along with the facility managers who decided how the training would be operated in their respective facilities. As a result, the differences between the approaches followed were minimized; one facility chose a different strategy and did not fall into either group. Furthermore, neither of the two approaches that we had initially envisioned was carried out as planned. The traditional training approach was conducted on-site rather than offsite in a “hotel”-style training, and the OTJ was ultimately more of a modular training approach. In addition, within each group of facilities (traditional and modular) the way training was carried out varied significantly; the supportiveness of facility managers and capacity of MTs also varied significantly. This is an important challenge that any program or country wishing to sustainably scale up with limited resources will need to consider.
Finally, classic limitations come with key informant interviews, observations, and small sample sizes. These limitations include bias from a potentially non-representative sample, courtesy bias (tendency of supervisees or participants to respond positively when asked about facility managers or about an activity sponsored by the organization doing the interviews), Hawthorne effect (the tendency to change or improve practices when being observed), as well as inter-rater reliability and subjectivity (different observers may consider practices differently). Some of these have been addressed to an extent through training and orientation of data collectors; however, they are important to keep in mind.
Discussion
The impact of malnutrition globally continues to have implications for the health, social, and economic development of many countries (UNICEF 2013). Malnutrition and childhood disease are intimately related. Malnutrition can contribute to a compromised immune response and greater susceptibility to disease, while disease can contribute to increased energy requirements, poor absorption of nutrients, anorexia, and greater susceptibility to malnutrition (Victora et al. 2008; Black et al. 2008). Emerging evidence suggests that this relationship extends well beyond childhood; malnourished children appear to be more susceptible to diet-related chronic disease later in life (Black et al. 2013; Adair et al. 2013). Undernutrition, particularly during early life, has been associated with the intergenerational cycle of malnutrition. This cycle consists of a malnourished mother being more likely to deliver an undernourished infant; in turn, that infant is more likely to grow to be an undernourished adolescent and adult.
For people living with diseases such as the human immunodeficiency virus (HIV) or tuberculosis (TB), the impact of malnutrition is further compounded. These illnesses not only increase nutritional requirements, but combined with declining immunity and reduced absorption and use of nutrients, they contribute to an accelerating cycle of poor health (de Pee et al. 2010). It is well established that HIV compromises the nutritional status of infected individuals, thereby worsening the disease’s effects. Likewise, good nutrition helps PLHIV to manage symptoms and opportunistic infections. Conversely, poor nutrition places PLHIV at increased susceptibility for infection. For infants, poor feeding practices, particularly during the first six months of life, place babies born to HIV-positive mothers at risk of becoming infected.
Evidence-based nutrition interventions exist that can positively impact maternal and child nutrition and significantly reduce mortality, if sufficient programmatic coverage is achieved (Bhutta et al. 2013). These interventions are relevant along the reproductive lifecycle for adolescent girls, women of reproductive age and pregnant women, neonates, and infants and children. They include family planning, psychosocial services, multiple micronutrient supplementation, tobacco cessation, delayed cord clamping, early initiation of breastfeeding and exclusive breastfeeding, vitamin K administration, kangaroo mother care, and complementary feeding (Bhutta et al. 2013). Over the past decade, strengthening nutrition interventions as part of health systems has been increasingly recognized as imperative for the prevention and treatment of malnutrition for all, especially for pregnant and lactating women, infants and young children, and people living with diseases such as HIV and TB (Bhutta et al. 2008; Bryce et al. 2008). Integrating these evidence-based nutrition interventions into health services is critically important.
In Haiti, as in many developing countries, health facilities are perennially understaffed, underqualified, and resource constrained. Capacity to implement high-impact nutrition interventions is inadequate. According to the World Health Organization (WHO), “critical shortages, inadequate skill mix and uneven geographical distribution of the health workforce pose major barriers to achieving the health-related Millennium Development Goals” (2010a) With WHO’s minimum threshold of 23 doctors, nurses, and midwives per 10,000 population for delivering essential maternal and child health services, Haiti is nearly off the charts. In 2010, Haiti only had five doctors, nurses, and midwives per 10,000 people (WHO 2010b).
Effective and high-quality capacity building of health care workers (HCWs) is needed to achieve sufficient programmatic coverage of proven nutrition interventions, to ensure the quality of nutrition services (assessment, counseling, and support) provided, and to increase HCW motivation and retention (Healthy Child Uganda 2011; Kennedy 1991). Unfortunately, the effectiveness of the various approaches to building capacity is unknown. There is a dearth of evidence to indicate which training approach is most effective for building the capacity and improving the quality of nutrition services.
Success of HCW trainings is typically determined based on knowledge and skills acquired and services improved. However, a number of factors affect human performance, including knowledge, skills, and capacity; attitudes and motives (internal); data and information; tools and resources; setting; and incentives (external). What we found represents an important contribution to the literature.
Knowledge, skills, and capacity: Pre- and post-training tests indicate that trainees learned the IYCF and NACS content. Feedback from trainees confirmed that MTs understood and effectively conveyed technical content. External factors described in greater detail below prevented trainees from putting knowledge fully into practice.
Attitudes and motives (internal): Trainees from traditional facilities were more likely to report that the topic was very useful (93 percent) compared with those from facilities following the modular training approach (64 percent) and those following the abbreviated training (57 percent). Similarly, trainees from traditional training facilities found more benefit from the training. This may well have to do with the fact that a higher number of trainees did not complete the training in facilities following the modular training approach. They might not have been as satisfied with the training or gotten as much out of the training. Therefore, the results regarding satisfaction may be biased against the modular training approach.
Data and information: Unfortunately, little was ascertained from the follow-up data collection regarding the data and information available to HCWs. However, almost all of those interviewed reported receiving little to no feedback on his or her performance of nutrition services. While HCWs may have learned and started off by doing things in an improved way, if follow-up is not enacted to reinforce good practices, after a while people can go back to old habits.
Tools and resources: Facility support, client-provider ratios, and availability of equipment and supplies were probably the biggest factors affecting the quality of nutrition services delivered. And, while trainings certainly are necessary, the capacity of MTs and participant selection probably mattered more than the approach (traditional versus modular).
Setting: A revealing finding was that trainees from traditional training facilities reported more opportunities to practice the new knowledge or skills during the training than those in facilities following the modular or abbreviated training approach. This is contrary to what one would have expected of the modular approach that was intended to involve on-the-job training (OJT) that, by its very definition, serves as an opportunity to practice. This finding may reflect more on the time allocated to the training sessions and their overloaded nature. It may also have to do with facility managers rarely permitting MTs to take time away from their normal duties to coach trainees outside of the formal training sessions. Facility managers rarely reduced the workload of MTs in modular training facilities. Instead, they were expected to squeeze the training into the work day after normal consultation hours, so time to practice new skills was reduced or eliminated.
Incentives (external): We found that many facilities were no longer maintaining or completing the columns related to nutritional status in the registers. This underscores concerns raised regarding facilities being understaffed and HCWs being overworked and therefore unable to provide the full range of nutrition services. Similarly, while respondents (trainers and trainees) commented on improvements in nutrition counseling after the training, during observations, providers demonstrated almost none of the priority skills. This also may have to do with a lack of time or personnel to provide nutrition counseling. Given the reliance of many facilities on social service residents, it is also possible that HCWs observed working in the priority units of the health facilities during follow-up data collection may not have participated in the training.
Conclusions and Recommendations
One important finding was that the differences between the two approaches selected and followed by the health facilities were fewer than originally anticipated. For instance, all trainings were conducted on-site (in the facilities), and all trainers were staff from the facilities. This meant that all trainees had the potential to be coached. While training on-site had its advantages (increased participation) it also resulted in greater potential for trainees to be called to work, disrupting the training and learning process. Trainers noted this as a major challenge.
We were able to participate in the training…without stopping our regular work…I was still accessible to the hospital and to my patients.
—Trainee, Nurse, Pediatric Unit
Unexpectedly, but perhaps not surprisingly given the severe human resource shortages many health facilities in Haiti face, HCWs were sometimes selected out of convenience or availability rather than for more strategic reasons such as relevance or interest. Those HCWs who might have been best placed to put knowledge into practice or to make significant shifts in routine services provided often could not be spared and, therefore, did not always participate in the training. This was observed in both facilities types but more so in the traditional training facilities. In these facilities, colleagues and patients who struggled during the busy morning hours of consultation felt the HCWs’ absence more acutely.
Although differences were somewhat fewer than expected, the findings indicate that trainees liked the modular training approach better, and the approach carried less of a financial or opportunity cost for facilities and facility staff. While all trainings did occur on-site (in the facilities) and provided some amount of opportunity to put knowledge into practice, where the modular training approach was followed, trainees had increased opportunities for immediate practice of skills attained. Staff enrollment also was higher in modular training facilities because participants did not have to miss a full week of work to participate.
Some unique challenges also appeared in this approach. In particular, it was difficult to ensure that trainees attended all modular training sessions. It was difficult to ensure attendance over the course of numerous sessions and weeks because of staff rotations and turnover.
Finally, although none of those interviewed mentioned costs of the trainings borne by patients, they did comment on being distracted by participants frequently leaving the training to attend to patients. The implication of this distraction is a “cost” to patients who most likely faced longer wait times (particularly in understaffed units of the health facilities) while HCWs were being trained.
Given the realities on the ground in Haiti, including limited human (within the SPRING/Haiti team and at the health facilities) and financial resources, all facilities experienced similar challenges affecting the effectiveness of the training provided on nutrition services. Staff members are expected to add NACS services to their routine services. However, they are already overworked. Without additional staff or staff clients to nutrition support services, it may be challenging—if not impossible—to achieve full coverage of NACS services at the facility level.
Based on these findings, we feel strongly that strengthening the overall systems to better integrate nutrition services would have the greatest impact. To do this, ministries of health would need to define and implement—
- nutrition standards of care and priority elements for each level of the health system
- human resources necessary – quantity and levels – for providing those standards of care at each level
- specific training needs (content, duration, pre-service vs. in-service vs. refresher, methodology) of each cadre or role within health facilities at each level)
- a data-driven quality improvement (QI) approach to service delivery that continuously identifies and addresses barriers to the delivery of the standards of care.
We recommend that governments and projects take the following actions, if and when in-service training is deemed appropriate. These steps will help to cautiously amplify the use of modular training approaches with shorter training sessions rolled out over an extended period of time.
- Take proactive steps to fully orient, encourage ownership, and gain support for the trainings among facility managers to ensure the proper selection of trainers and trainees and to increase the material and “moral” support often needed for a successful training. This could be accomplished through more in-depth and strategic orientations for facility or unit managers (directors and administrators).
- Before a TOT, it is important to engage the facility managers in a workshop to develop a vision for improved nutritional support services and to teach them to use data to monitor changes in performance of nutritional service-related tasks.
- Prioritize documentation of training processes and analysis comparing various approaches. Without great effort or cost, process monitoring and analysis can be integrated into routine monitoring (using existing information systems) or supervision.
- Be strategic in the selection of trainers and trainees both in terms of applicability of content to daily work (i.e., those who work in prenatal, pediatric, or HIV units) and motivation/interest in the topic.
- Train HCWs in what they can realistically do given existing equipment and infrastructure and time/workload.
- Consider carefully the timing of trainings (days of the week and hours of the day), so they are least disruptive to client flow and the normal functions of HCWs.
- Emphasize the ELC more during future TOTs, encouraging trainers to build on what trainees know already and providing adequate time to practice counseling skills during the trainings.
- Ensure the provision of an adequate space for the training, stand for flip charts, a projector, and energy source to run the projector.
- Adjust the workload of trainers (health facility staff) or other facility staff to allow time for adequate preparation for, implementation of, and follow-up to the training (i.e., coaching). The latter is a valuable aspect of the OJT approach, which overworked trainers often neglect.
- Incentivize trainees to participate in all training sessions for the entirety of each session. This could be done by having participation in trainings be reflected as a positive thing in their performance reviews.
Footnotes
1 To be considered “trained,” trainees had to complete the pre- and post-training tests.
2 Completion of the training was defined as having completed the post-training test.
3 iSanté data were not available for Hôpital Sainte Thérèse de Hinche, a traditional training facility, as well as Hôpital Maternité Isaie Jeanty, the facility that followed the abbreviated training approach.
References
Adair, Linda S., Caroline H.D. Fall, Clive Osmond, Aryeh D. Stein, Reynaldo Martorell, Manuel Ramirez-Zea, Harshpal Singh Sachdev, et al. 2013. “Associations of Linear Growth and Relative Weight Gain During Early Life with Adult Health and Human Capital in Countries of Low and Middle Income: Findings from Five Birth Cohort Studies.” The Lancet 382 (9891) (August): 525–534. doi:10.1016/S0140-6736(13)60103-8.
Alipour, M. 2009. A study on the job training effectiveness: Empirical evidence of Iran. International Journal of Business and Management. 4(11): 63-68.
Bhutta , Z., Das, J., Rizvi, A., et al. 2013. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? The Lancet. 382: 452-477.
Black, Robert E., Cesar G. Victora, Susan P. Walker, Zulfiqar A. Bhutta, Parul Christian, Mercedes de Onis, Majid Ezzati, et al. 2013. “Maternal and Child Undernutrition and Overweight in Low-income and Middle-income Countries.” The Lancet 382 (9890) (August): 427–451. doi:10.1016/S0140-6736(13)60937-X.
Black, Robert E., Lindsay H. Allen, Zulfiqar A. Bhutta, Laura E. Caulfield, Mercedes de Onis, Majid Ezzati, Colin Mathers, and Juan Rivera. 2008. “Maternal and Child Undernutrition: Global and Regional Exposures and Health Consequences.” The Lancet 371 (9608) (January): 243–260. doi:10.1016/S0140-6736(07)61690-0.
Crist, K. (2006). Environmental Vulnerability in Haiti. The Wilson Center. Retrieved from: http://www.wilsoncenter.org/event/environmental-vulnerability-haiti
De Pee, Saskia; Semba, Richard D. 2010. “Role of nutrition in HIV infection: Review of evidence for more effective programming in resource-limited settings.” Food and Nutrition Bulletin 31 (Supplement 4) (December): 313S-344S (32).
Felling, B. 2013. Personal Communication. Supply Chains for Community Case Management.
Healthy Child Uganda. 2011. Community Health Workers and Community Case Management: Policies and Progress in Uganda within a Global Context. Retrieved from, http://www.healthychilduganda.org/media/Community-Health-Workers-and-Community-Case-Management-April-2011.pdf
Hiner C., Mandel B., Weaver M., Bruce D., Lee P., McGaw B., McLaughlin R., Anderson J. 2009. “Evaluation of a voluntary counseling and testing training program in the Caribbean region.” Human Resources for Health. 2009; 11:11.
Jiskoot, P. 2008. “On the job training of clinical officers in Malawi.” Malawi Medical Journal. 20(3):74-77.
Kennedy, E. 1991. Successful Nutrition Programs in Africa: What Makes Them Work? Washington DC: World Bank.
Ministry of Public Health and Population [le Ministère de la Santé Publique and de la Population] (MSPP), Haitian Childhood Institute [l’Institut Haïtien de l’Enfance] (IHE) and ICF International. 2013. 2012 Haïti Mortality, Morbidity, and Service Utilization Survey: Key Findings. Calverton, Maryland, USA: MSPP, IHE, and ICF International.
Ozek, B., Saat, Z., Temiz, AT., Kinzie, B. 1998. “On-the-Job Training Follow-up Visits to Improve the Quality of Family Planning Services.” European Journal Contraception and Reproductive Health Care. Dec; 3 (4): 201-6.
Riding, R., Mortimer, J. 2000. “A study of the on-the-job training of production line operatives in manufacturing companies.” International Journal of Training and Development. 4:2.
Supply Chains for Community Case Management. 2013. Training health extension workers in the integrated pharmaceutical logistics systems. Arlington, Va.: Supply Chains for Community Case Management.
Tobias C.R., Downes A., Eddens S., Ruiz J. 2012. “Building Blocks for Peer Success: Lessons Learned from a Train-the-Trainer Program.” AIDS Patient Care and STDs. 2012;13(1):53–59.
UNICEF. 2013. “Improving Child Nutrition: The achievable imperative for global progress.” Available at: http://www.unicef.org/publications/files/Nutrition_Report_final_lo_res_8_April.pdf
USAID | DELIVER PROJECT. Task Order 1. 2007. Supervision and On-the-Job Training for Supply Chain Management at the Health Facility. Arlington, Va.: USAID | DELIVER PROJECT, Task Order 1.
Victora, Cesar G., Linda Adair, Caroline Fall, Pedro C. Hallal, Reynaldo Martorell, Linda Richter, and Harshpal Singh Sachdev. 2008. “Maternal and Child Undernutrition: Consequences for Adult Health and Human Capital.” The Lancet 371 (9609) (January): 340–357. doi:10.1016/S0140-6736(07)61692-4.
World Food Programme (WFP). 2014. Haiti Overview. Retrieved from, http://www.wfp.org/countries/haiti/overview
World Health Organization. 2010a. Achieving the health-related MDGs. It takes a workforce! Retrieved from: http://apps.who.int/globalatlas/default.asp
_______ (2010b). WHO’s Communicable Disease Global Atlas. Retrieved from: http://apps.who.int/globalatlas/default.asp
Appendices
To view the appendices please use the download link at the top of the page.