A Report on the Key Findings of the Formative Research Conducted at the Initiation of the Project in 2012

Executive Summary
SPRING is working in India in collaboration with Digital Green, a U.S.- and India-based organization, spreading across 30 villages in the Keonjhar district of Odisha state. This collaboration focuses on adapting Digital Green’s innovative community media model to address nutrition in the first 1,000 days, reaching new audiences through mobile video screenings and facilitated discussions, with adoption of key behaviors verified through home visits.
In November 2012, SPRING and Digital Green completed a qualitative study in purposely selected villages in Keonjhar district to identify current social and cultural determinants, practices, and knowledge on maternal, infant, and young child nutrition (MIYCN). The information was collected to help guide the development of community-based videos promoting optimal nutrition practices to improve the nutritional status of pregnant and lactating women and young children.
The specific objectives of the qualitative research were to:
- Identify existing family relationships in terms of decision making. (Who makes decisions regarding nutrition? Who makes decisions regarding health? What are some of the relationships linked to gender and/or caste?)
- Identify the current MIYCN practices and barriers that need to be addressed, such as food misconceptions (taboos); knowledge related to the nutrition and health of pregnant and breastfeeding women and children under two years of age; and influencing individuals.
- Identify the major nutritional issues adolescent girls and women face, including societal structures, taboos, barriers, as well as promising practices to build upon.
- Understand the current hygiene practices with a focus on handwashing with soap.
- Identify sources of information currently used by adolescents, pregnant women, and breastfeeding mothers, and also how current services and providers are perceived (Integrated Childhood Development Services [ICDS], Anganwadi workers [AWWs], accredited social health activists [ASHAs], and auxiliary nurse midwives [ANMs]).
- Identify the perceptions of community members and video production and dissemination teams regarding the Digital Green videos.
This report is comprised of five distinct parts: Part 1 presents the current nutrition situation in India; part 2 reviews the formative research methodology; part 3 shares the key findings of this qualitative study; part 4 is a discussion of those findings; and part 5 summarizes the conclusions and recommendations.
Summary of Findings
As identified in this formative research, many factors affect optimal MIYCN practices in Keonjhar district, underscoring the fact that improving MIYCN practices goes far beyond increasing knowledge. These factors include the following:
- Many women have limited agency to decide when to eat, how much to eat, or when to rest, due in part to the traditional gender-related social norms. It is key to get a better understanding of how to ensure that breastfeeding mothers have enough food to eat while breastfeeding and have access to a healthy diversity of foods.
- Family organizational structures can also create confusion, especially when a mother-in-law’s advice contradicts that of the ASHAs and AWWs.
- Although lack of knowledge of optimal MIYCN practices is not the clear driver behind current MIYCN behaviors, this research indicates that there are areas where knowledge, information sharing, and skills need to be strengthened, such as exclusive breastfeeding and complementary feeding.
- It is important to reiterate that there are many traditional practices and food taboos (some harmful and some essentially harmless or neutral) that dictate what women can eat while they are breastfeeding, specifically for the first six months of the life of the child.
- Another important consideration for prioritizing nutrition video content is the strongly held belief that iron–folic acid (IFA) supplements, if taken during pregnancy, lead to bigger babies, with negative consequences. With high rates of anemia in India, this is a key misconception to address.
- Health workers are critical in supporting optimal nutrition for women and children; at times they are trusted by the community but at other times they are not. Some AWWs are perceived as actually using some of the government schemes for their own benefit. The ASHAs can be a reliable source of information but only if they provide outreach services.
Key Recommendations
The research was also able to highlight key behaviors that seem “ripe for change” and that could be further explored through the development and use of community videos:
- Promoting exclusive breastfeeding during the first six months of life, explaining that breast milk provides sufficient liquid to the baby even during the hot months; that women make more milk when the child breastfeeds; and that when a child is ill, she/he needs to be breastfed more often.
- Promoting the health of breastfeeding mothers while encouraging the reduction of women’s workload during pregnancy and breastfeeding.
- Developing videos that address nutrition-related issues focused on the first 1,000 days and strengthening support for mother/child pairs following the first 21 days.
- Addressing maternal nutrition during pregnancy and postpartum (promoting iron-rich foods), promoting one extra meal, promoting rest, and strengthening adherence to recommended IFA supplementation by addressing some of the misconceptions identified (e.g., the fear of having too big a child).
- Developing videos teaching mothers about how critical complementary foods are and how to improve their quality with locally grown foods.
- Strengthening the role of husbands and fathers as supportive partners and engaging them in video viewing and discussions.
- Targeting mothers-in-law when developing nutrition videos, recognizing their roles in childcare practices, since they are powerful decision makers and gatekeepers in the households.
- Engaging community health agents (ASHAs and AWWs) in reviewing the content of the videos and perhaps featuring them as “stars” in the videos given their specific role in the community.
- Promoting handwashing with soap as a critical hygiene practice.
1. Introduction and Background
1.1 Overview of the SPRING/Digital Green Collaboration and Feasibility Study
SPRING is a five-year USAID-funded Cooperative Agreement to strengthen global and country efforts to scale up high-impact nutrition practices and policies and improve maternal and child nutrition outcomes, with a focus on the first 1,000 days. SPRING has committed to identifying and testing proven or highly promising social and behavior change communication (SBCC) tools and models to promote optimal maternal, infant, and young child nutrition (MIYCN). In October 2012, SPRING entered into a formal partnership with Digital Green, a U.S./India-based nongovernmental organization (NGO), to test the adaptation of an innovative “human-mediated digital learning approach” currently being used by Digital Green to promote the diffusion of improved agricultural practices.
In November 2012, SPRING and Digital Green completed a qualitative study in purposely selected villages in Keonjhar district to identify current social and cultural determinants, practices, and knowledge on MIYCN. The research findings also informed the development of a community nutrition training package for use in sensitizing a range of community agents involved in the production of context-specific nutrition and hygiene-focused video content. Furthermore, the aim of the SPRING/Digital Green collaboration and qualitative study was to establish whether or not the current Digital Green agricultural extension platform could be adapted for nutrition content, and to document the process for use in other settings. The nutrition-focused videos feature mothers and other community members, speaking in their own language, about their individual experiences with selected key nutrition and hygiene practices. The approach uses a “dialogue” or “reflective” process among peers, rather than a traditional nutrition education approach of outside “experts” informing clients. When possible, the approach uses positive deviants from the communities who are already practicing the recommended behaviors as the main actors for the videos. Data on intention to adopt and verification of adoptions or promotions of key behaviors are then collected and organized using a near-real-time analytical dashboard, which facilitates informed decision making and the improved design of subsequent videos.
The adaptation of the Digital Green model was piloted in 30 villages in two blocks of Keonjhar district of Odisha state: Patna and Gartageon. This pilot was also supported by the Voluntary Association for Rural Reconstruction and Appropriate Technology (VARRAT), the local community-development NGO partner working with Digital Green in Odisha.
1.2 Maternal and Child Health and Nutrition Situation in India
Although India is among the top five countries in terms of absolute numbers of maternal deaths, encouraging progress has been made in reducing the burden of maternal and child death. During the last decade, child mortality rates have dropped by 45 percent in India. In 1990, when the global under-five mortality rate was 88 per 1,000 live births, India also carried a high burden of child mortality: 115 per 1,000 live births (Office of Registrar General, 2013). Two decades later, in 2010, India’s child’s mortality rate of 59 per 1,000 live births was close to the global average of 57. At the national level, the maternal mortality ratio (MMR) dropped from 212 maternal deaths per 100,000 live births in 2007–2009 to 178 in 2010–2012, a decline of 16 percent (Maternal Mortality Bulletin 2013). Nevertheless, much remains to be done to improve child and maternal health and survival in India. There are still 56,000 maternal deaths each year and about two-thirds of these occur in six states, one of which is Odisha. With the current under-five mortality rate, about 1,580,000 children in India do not reach their fifth birthday. Of these, 56 percent of children die in the first month of life (880,000 children), and 79 percent (1,250,000) die within their first year, including the neonatal period (Ministry of Health and Family Welfare, January 2013).
In terms of nutrition, of the 150 million undernourished children worldwide, more than one-third live in India (UNICEF 2013). The most recent National Family Health Survey (NFHS-3), conducted in 2005–2006, indicates that 48 percent of children under five are stunted and 20 percent of children under five are severely malnourished, as measured by wasting (IIPS and Macro International 2007). The prevalence of wasting in India is twice as high as the average prevalence in sub-Saharan Africa and seven of 10 children in India are anemic. Undernutrition occurring in the first two years of life is particularly difficult to overcome later in life. The NFHS-3 survey data show that during the first six months of life 20–30 percent of Indian children exhibit signs of undernutrition, peaking at 20 months of age (IIPS and Macro International 2007). In India, 56 percent of severe wasting occurs before a child reaches the age of two years, which underscores the importance of adequate nutrition in the first 1,000 days of a child’s life (Coalition for Sustainable Nutrition Security in India 2008). Figure 1 shows the weight-for-age and height-for-age of Indian children through 35 months of age, illustrating the severe nutritional deficits that occur in this critical window.
In India, one-third to one-half of child deaths can be attributed to undernutrition (Naandi Foundation 2011). When not resulting in child deaths, undernutrition causes stunted physical growth and cognitive development, deficits that result in economic losses equivalent to an estimated 3 percent annually of the country’s gross domestic product (GDP) (Naandi Foundation 2011).
Figure 1: Weight-for-age and height-for-age, Indian children up to 35 months of age
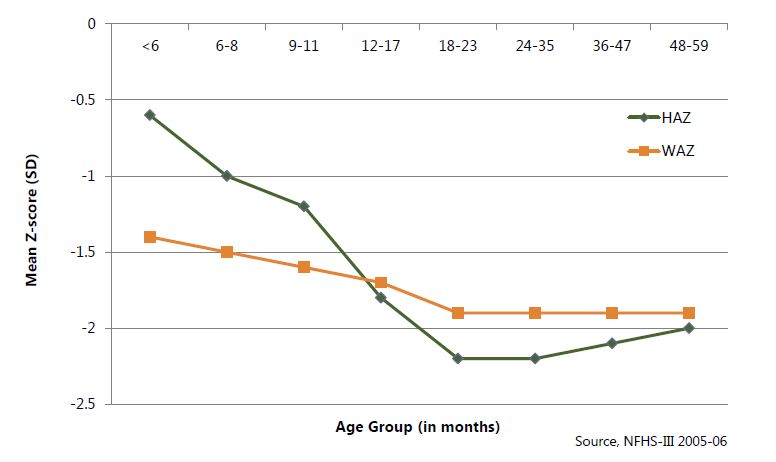
Source: IIPS and Macro International 2007
Additionally, among underweight women, 44 percent are moderately to severely underweight.
Anemia in India
Globally, India ranks high in the prevalence of anemia, with a national prevalence of 74.3 percent, making it a severe public health problem (WHO n.d.). Fifty-nine percent of pregnant women in India are anemic, and it is estimated globally that anemia is the underlying cause for 20–40 percent of maternal deaths (Viteri 1994). The NFHS-3 shows that anemia is widely prevalent among all age groups, as illustrated in Table 1. The prevalence of anemia among adolescent girls (Hb < 12 g/dl) and boys (Hb < 13 g/dl) is alarmingly high; with girls being most at risk (56 percent of adolescent girls aged 15–19 years versus 30 percent of boys aged 15–19 years). Anemia prevalence among children aged 6–35 months has actually increased between the two most recent NFHS surveys from 74.3 percent (NFHS-2) to 78.9 percent (NFHS-3), indicating that seven of 10 children aged 6–59 months in India is anemic (IIPS and Macro International 2007).
Table 1: Prevalence of Anemia among Different Age Groups in India
| Age Group | Prevalence of Anemia (Percentage) |
|---|---|
| Adolescent Girls | |
| Children (6–35 months) | 78.9 |
| Children (6–59 months) | 69.5 |
| All women (15–49 years) | 55.3 |
| Ever-married women (15–49 years) | 56.0 |
| Pregnant women (15–49 years) | 58.7 |
| Lactating women (15–49 years) | 63.2 |
| 12–14 years | 68.6 |
| 15–17 years | 69.7 |
| 15–19 years | 55.8 |
Source: IIPS and Macro International 2007
Undernutrition in Odisha
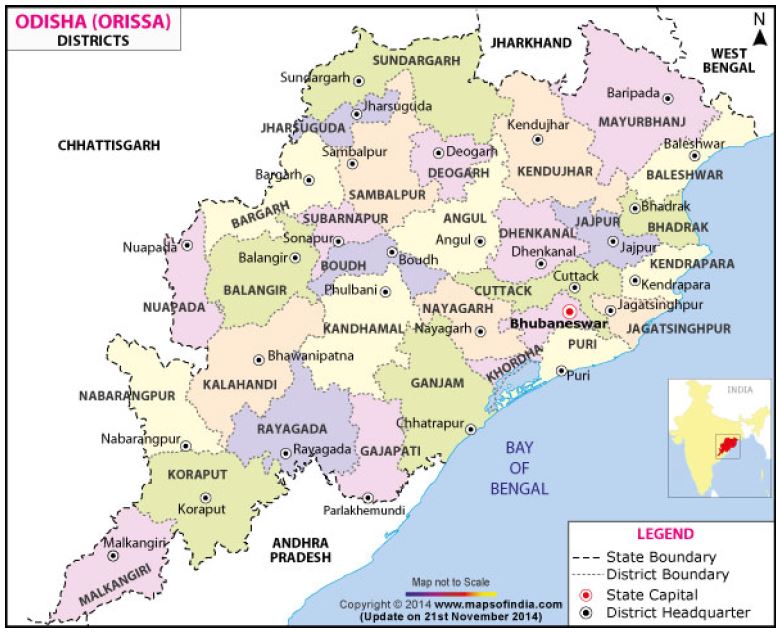
On the eastern coast of India lies Odisha, one of the country’s least-urbanized states (Figure 2). In the last few decades, however, the state has benefited from growing industrialization, with an average income that has almost tripled; however, Odisha has the highest percentage of its population living below the poverty line among all India states (UNICEF 2012). Odisha’s per capita income and household income are significantly lower than the national averages. While average household income at the national level is 27,857 Indian rupees (INR), it is INR 16,500 in Odisha. The national average capita income is INR 5,999; in Odisha it is INR 3,450. Based on the percentage of rural population consuming less than 1,890 kilocalories per day, Odisha has moved from being classified as low food insecure (11.1 percent) in 1999–2000 to moderate food insecure (15.4 percent) in 2004–2005. In the same time period, national levels of food insecurity fell from 15.1 percent to 13.2 percent (MSSRF/WFP 2008).
Over 80 percent of the workforce in Odisha is employed in the agricultural sector, and 50 percent of the GDP of India comes from Odisha. Twenty percent of households in Odisha belong to a scheduled caste (SC), 23 percent to a scheduled tribe1 (ST), and 27 percent to other backward classes (OBCs) (IIPS and Macro International 2008).
Figure 2: Map of Odisha’s districts
Odisha’s infant and under-five mortality rates, at 65 and 91 per 1,000, respectively, are higher than the national averages. Despite declining rates in mortality in the past few decades, one in 11 children in Odisha will die before reaching the age of five (IIPS and Macro International 2008). As seen in Figure 3, children in Odisha, particularly children of STs, exhibit alarmingly high rates of undernutrition. Tribal groups in India are among the most underprivileged and comprise about 8 percent of the population. The STs in Odisha, also known as Adivasi (the Sanskrit word for indigenous) communities, have double the unemployment rate of non-Adivasi people, and only one-third of children from STs receives a primary education. Data indicate that nearly 75 percent of the tribal population in Odisha is below the official poverty line (Mehta 2011). Tribal communities characteristically have higher mortality and morbidity rates and poorer access to health services than non-Adivasi communities (IIPS and Macro International 2007, Ministry of Health and Family Welfare 2013). Children from STs are about 1.5 times more likely to die before their fifth birthdays than those from SCs (Mehta 2011). Nationally, 57 percent of ST children are malnourished, 28 percent are severely stunted, and 54 percent are underweight (Mehta 2011). In 2005–2006, under-five mortality rates for children from STs were almost twice as high as those of nontribal children. This under-five mortality rate was also 1.5 times higher than for children from SCs.
Figure 3: Children's nutritional status in Odisha
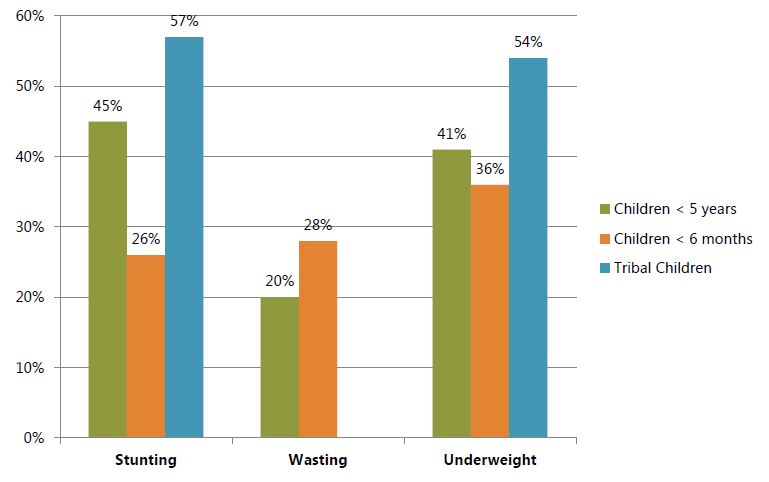
Source: IIPS and Macro International 2008
NFHS-3 shows that only one-half of the children under six months of age are exclusively breastfed, although the average breastfed child is breastfed for 34 months. Fifty-five percent of babies are put to the breast within the first hour of life to receive colostrum; however, there is a significant prevalence (42 percent) of supplemental feeding within the first few weeks of life. About 56 percent of children aged 6–23 months are fed the recommended minimum times per day, but only 44 percent are fed from the minimum number of food groups per WHO recommendations (IIPS and Macro International 2008). Anemia is a serious health issue in Odisha, with a prevalence rate among women of reproductive age at 62.8 percent, compared to the national average of 56.1 percent (Panigrahi and Sahoo 2011). Additionally, close to 65 percent of children 6–59 months in Odisha are anemic and this prevalence has risen since the previous NFHS (IIPS and Macro International 2008).
Health in Keonjhar District
The SPRING/Digital Green project site is located in Keonjhar district, which is comprised of 2,132 villages. Eighty percent of the population in Keonjhar lives in rural areas and engages in traditional agriculture, and more than three-quarters of the population live below the poverty line (Government of Odisha 2012). The infant mortality rate in Keonjhar is 58 per 1,000 live births, and the under-five mortality rate is listed at 85 per 1,000 live births in the latest official data (Ministry of Home Affairs 2011). Keonjhar has a high rate of undernutrition compared to other districts in the state, with moderate to severe undernutrition at a rate of 20.46 percent. Only 24.6 percent of children are exclusively breastfed for six months, meaning that the remaining almost 86 percent receive supplementation of breast milk with water and other fluids during the first six months. On average in the district, children are not fed vegetables or fruits until 8.5 months or solid foods categorized as “adult” foods until 9.4 months (Ministry of Home Affairs 2011).
2. Formative Research Methodology
2.1 Goal and Objectives
In November 2012, SPRING and Digital Green completed a qualitative study in purposely selected villages in Keonjhar district to identify current social and cultural determinants, practices, and knowledge on MIYCN. The information was collected to help guide the development of community-based videos promoting optimal practices to improve the nutritional status of pregnant and lactating women and young children, with a focus on the first 1,000 days. The specific objectives of the study were to:
- Identify existing family relationships in terms of decision making. (Who makes decisions regarding nutrition? Who makes decisions regarding health? What are some of the relationships linked to gender and/or caste?)
- Identify the current MIYCN practices and barriers that need to be addressed, such as food misconceptions (taboos); knowledge related to the nutrition and health of pregnant and breastfeeding women and children under two years of age; and influencing individuals.
- Identify the major nutritional issues adolescent girls and women face, including societal structures, taboos, barriers, as well as promising practices to build upon.
- Understand the current hygiene practices, with a focus on handwashing with soap.
- Identify sources of information currently used by adolescents, pregnant women, and breastfeeding mothers, and also how current services and providers are perceived (Integrated Childhood Development Services [ICDS], Anganwadi workers [AWWs], accredited social health activists [ASHAs], and auxiliary nurse midwives [ANMs]).
- Identify the perceptions of community members and video production and dissemination teams regarding the Digital Green videos.
2.2 Selection of Research Sites
For the formative research, a total of six villages (three in each block) were selected from the 30 priority villages that were selected to participate in the one-year feasibility study. The six villages were purposely selected based on the percentage of scheduled tribe. The population rate of STs in the program villages ranges from 100 percent to 40 percent; thus, three villages in each block were identified to represent this range: one village having a high ST population, one with a medium ST population, and one with a smaller ST population. In addition to representing the cultural diversity, these six villages were selected from various Gram Panchayats (village councils) to also capture information about Panchayat systems and their effectiveness. The team of researchers agreed to select villages where the Panchayat had already been actively addressing nutrition in their communities, as it was agreed from the start that the pilot would be conducted in villages that showed promising leadership in health promotion. Further, as the pilot was limited in time (one year), it needed to quickly show evidence indicating that integrating nutrition within an agricultural SBCC platform might be feasible. See Table 2 for names of selected villages for the qualitative research.
Table 2: Selected Villages for Formative Research in Kehonjar District, Odisha State, Including Percentage of Households from Scheduled Tribes
| Name of Block | Name of Panchayat | Name of Village |
|---|---|---|
| Patna | Dumuria | Baidabaja (100% ST) |
| Erendei | Begunakhaman (34% ST) | |
| Palanghati | Kumulabahali (71% ST) | |
| Ghatagaon | Santarapur | Chatia (74% ST) |
| Santarapur | Raghubeda (92% ST) | |
| Manoharpur | Gandasila (74% ST) |
2.3 Research Team
The nine-person research team was made up of lead researchers, including a Senior Nutrition Advisor from Save the Children India, the Nutrition Program Manager from Digital Green, a Global Advisor from Save the Children US, and key interviewers with extensive experience at the community level in agricultural, health, and social sciences. Interviewers were divided into three teams, with an equal gender representation on each team. Two of the teams were primarily responsible for conducting 12 focus group discussions (FGDs), while the Global Advisor conducted 16 in-depth interviews (IDIs) with the local NGO partner, VARRAT’s Program Director as a translator. SPRING trained the research teams on the objectives of the research, the tools, data collection, and recording of information. The data collection was conducted for four days in the field. At the end of each day, the teams met for two hours to debrief, highlight findings, and review questions or issues.
2.4 Research Methodology
The methodology was developed in collaboration and extensive consultation with the local partner (VARRAT), and Digital Green. The research protocol was submitted to the internal review board (IRB) at John Snow, Inc. (JSI), for approval and to ensure that the research objectives and tools met all ethics criteria and would not create harm for respondents and communities involved in the research. Expedited IRB approval was received under category 7 after a formal review of protocol and tools. The tools were developed in English and translated into Odia. All teams had native Odia speakers; the only person not speaking Odia was the Global Advisor, who worked with a translator.
Data collection was organized around two phases. During the first phase, in-depth interviews were conducted with key informants to inform the research questions and tools. Key informants included the Director of Programs of VARRAT, the UNICEF Regional Coordinator, one ANM, one AWW, and members of the VARRAT video production team.
The second phase included a mix of IDIs and FGDs, all conducted in Odia (Table 3). All participants signed consent forms before each FGD or IDI began. Extensive verbatim notes were taken in Odia and then translated into English. FGDs and IDIs were conducted with primary target respondents, secondary targets, and representatives of community systems. Specifically, the research included nine groups of participants:
- Pregnant women
- Breastfeeding women with children less than six months old
- Breastfeeding mothers of children between six months and two years old
- Mothers-in-law
- Fathers of children less than two years old
- VARRAT community service providers and other staff
- Anganwadi workers
- Nutrition Committee members
- Gram Panchayat leaders
Table 3: Summary of FGDs and IDIs Conducted during the Second Phase of Qualitative Research
| Focus Group Discussions: 6–15 People | No. Held |
|---|---|
| In-Depth Interviews | |
| Pregnant women | 2 |
| Breastfeeding mothers/child < 6 months | 2 |
| Breastfeeding mothers/child 6 months to 2 years | 2 |
| Mothers-in-law/grandchildren < 2 years | 1 |
| VARRAT community service persons | 1 |
| Anganwadi worker | 1 |
| Village Health Committee member | 1 |
| Nutrition Committee | 1 |
| Gram Panchayat leader | 1 |
| Pregnant women | 4 |
| Breastfeeding mothers/child < 6 months | 4 |
| Breastfeeding mothers/child 6 months to 2 years | 4 |
| Fathers/children < 2 years | 4 |
| Director of Programs, VARRAT | 1 |
| UNICEF Regional Coordinator | 1 |
| Auxiliary nurse midwife | 1 |
| Anganwadi worker | 1 |
| Members of the VARRAT video production team | 1 |
3. Study Findings
The research findings have been organized by the six specific objectives outlined for the study.
3.1 Objective 1: Identify Existing Family Relationships in Terms of Decision Making
FGDs and IDIs were conducted with pregnant women, lactating mothers, mothers-in-law, and husbands to understand how families are organized, and which individuals in the family are decision makers, gatekeepers, and/or influencers to target for the promotion of key behaviors. From the interviews, it is clear that most families provide a source of comfort and support to women and children and ensure that children are never left alone, even though women have to go back to work very soon after giving birth. The families interviewed are clearly organized around some power and labor sharing responsibilities and are both a source of support and advice, though at times erroneous. Additionally, it was evident that the dynamics within families are evolving in India. This research focused on villages within a traditional rural setting in Keonjhar, but even in this setting, an increasing number of women have access to education, which is influencing women’s agency and decision making regarding their health and children. The Government of India (GoI) is also focusing on strengthening primary care systems and community health programs to ensure that families have access to education and services at the community level—so, although family members play an important role in deciding what women and children eat, community health workers such as ASHAs, AWWs, and ANMs are playing an increasing role in building understanding among families about optimal MIYCN practices.
3.1.1 Role of Mothers-in-Laws (Sassous): A Source of Authority, Expert Advice, and Support
In traditional Indian culture, after marriage, many women live with their husband’s parents, and at times with their husband’s brothers and their wives. It is not unusual to see nine to 12 people across three generations living under one roof. During the IDIs and FGDs, most women, including pregnant women, breastfeeding mothers, and mothers-in-law, reported that their families were organized around this extended pattern, where daughters-in-law move in with the husband’s parents. Both sets of respondents (mothers-in-law and pregnant and lactating women) shared that within this extended family structure, there is a nonformal division of labor; that this structure provides support to pregnant women and women who have just given birth; and where mothers-in-law and elderly parents play an active child caring role while the younger generation goes back to work in the fields.
In terms of labor distribution in the household, usually the youngest daughter-in-law has an overwhelming burden of work. She is expected to cook and serve meals, and in most cases eats last, after everyone else has been fed. All pregnant and breastfeeding mothers reported that they really don’t have any decision-making power within the extended household, and that their mother-in-law is the one who makes decisions for them. However, for most of the respondents, they also shared that they trusted the advice of their mother-in-law, as someone with years of experience raising families. The mother-in-laws were seen as the main authority, a source of expert advice and support to the other women and children in the family, playing an active role in organizing the labor distribution within the home.
My mother-in-law is very good. I did not feel frightened when I was in the hospital as my mother-in-law was there. My mother-in-law supports me the most. She helps me with cooking and cleaning utensils.
-IDI with mother with child less than six months old
The caregiver of the lactating mother is very powerful, it is usually the mother-in-law and husband, but the mother-in-law is more powerful than the husband. The mother-in-law is the primary caregiver of the pregnant and lactating mother. The mother-in-law is usually preparing the food for the lactating mother when she returns home.
-KII [key informant interview] with ANM
3.1.2 Role of Mothers-in-Law Specifically Related to Nutrition during Pregnancy and Also for Infant and Young Child Feeding Practices
Many pregnant women and breastfeeding women reported that at first they were not sure what to eat during their pregnancy and postpartum period. They reported following the guidance of their mother-in-law in terms of deciding which foods they should eat while pregnant and when breastfeeding the new child. Many pregnant women reported that their mother-in-law decides which foods they can eat during pregnancy, and more importantly, it appears from the interviews that mothers-in-law decide what lactating mothers can eat until the time the child crawls.
Many pregnant and breastfeeding mothers reported trusting their mother-in-law and seeking her advice for rearing their children, specifically in terms of feeding the infant and young child. Others reported, however, that times were changing and that they, themselves, decided what to eat. Although in many households mothers-in-law appear to decide what pregnant and new mothers eat, one has to also take into consideration that many young women are seeking advice from others, such as ASHAs and ANMs, in caring for themselves and their children.
My mother-in-law decides what I can eat, and how often. My mother-in-law tells me the child will get sick if I eat different foods. If I eat more, she says I cannot digest the food and the child will have digestive problems. I believe my mother-in-law, I won’t be able to digest the food. I believe my mother-in-law, she knows. I will tell my children this later when I am a mother-in-law.
-IDI with mother with child less than six months old
My mother-in-law told me to take two meals a day because the baby eats small amounts, since the baby is small. When the baby grew a bit more, then my mother-in-law said I could eat more times, three times a day.
-FGD with mothers of children less than six months old
During the first month, I can only eat twice a day, once in the morning and once in the evening. At first, I feel hungry, but then it becomes a practice. There is a ritual, this is part of my family, it takes three to five days to get used to the food and being hungry, it takes some days to settle, but even if we are hungry we cannot do anything, this is what is decided by the elders. [What does your husband think?] He goes by his mother. This is a family tradition.
-IDI with mother with child less than six months old
I don’t know what to do but the elders tell me what to do and I do what they say to do. The elders tell me what to eat. Everyone says I need to eat the tablets [referring to iron folate tablets], so I eat the tablets. I take them and go to sleep so I have no problem with the tablets.
-IDI with pregnant woman
Mothers-in-law reported that their role is to support their daughters-in-law, as they have been mothers before and know from previous experience what women and children require to remain healthy. Mothers-in-law reported that they give nutritional advice to the pregnant and lactating mothers and they are trusted within the home, because they have experience. However, during the FGD discussion with mothers-in-law, it was clear that mothers-in-laws’ beliefs differ, with some stating that pregnant and breastfeeding mothers need to eat less to ensure that the new baby does not grow too big or to ensure that the breastfeeding baby can digest the food the mother eats. Some mothers-in-law reported fearing that “taking the IFA would make the baby too big for delivery.” Others reported that pregnant and breastfeeding mothers should eat more often and take their IFA regularly.
Pregnant women should eat more so that it would help the child be stronger and better. Yes, it is better for them to eat more, and also to take the good tablets from the hospital.
-FGD with mothers-in-law
All of the mothers-in-law during the FGD reported that some foods (referred to as “cold foods”), when consumed while breastfeeding the child, might make the child sick. They also reported that ripe raw papaya, okra, and white eggplant, if consumed by the lactating mother before the child is six months of age, would give a cold to the child.
Similar beliefs exist about certain foods that can give the baby a fever.
My mother-in-law tells me that I cannot eat other foods, because if I eat them the body of the baby will get hot, the baby will have a fever.
-IDI with mother with child less than six months old
It is also important to note that although all mothers-in-law reported that their daughters-in-law were exclusively breastfeeding, when probed, they explained that in fact the newborn received some additional liquids, or foods, based on traditions. The mothers-in-law listed honey, gripe water, and cow’s milk as expected to be given to the newborn when visitors come to welcome the new child.
3.1.3 Role of Mothers-in-Law Regarding Delivery and Postpartum Care
In addition to giving advice to pregnant women within their households, mothers-in-law play a critical role in decisions around delivery and postpartum care. It appears from the interviews that although ASHAs and ANMs are consulted during the pregnancy, the final decision for delivery is made in consultation with the mother-in-law. During the FGD with mothers-in-law, three of four reported that they knew that hospital delivery is better but they also shared that they felt that nowadays women go to the health center to deliver as they don’t know how to endure pain. “Woman go to the clinic as soon as there is pain.” Although the mothers-in-law did not clearly state that enduring pain can be a sign of pride for the household, they did report that “in [their] times [they] delivered at home and could endure the pain.” Although there is a need for more research, mothers-in-law might also be influencing where women give birth. Many of the lactating mothers interviewed reported having given birth at home.
The baby was born at home. This is my first baby, home is good. Lots of people in my family talked about where the baby would be born. My mother-in-law decided where the baby would be born.
-IDI with woman with child less than six months old
Once the child is born, new mothers who deliver at the clinic often come back the same day to the house. They are generally confined to one room in the house for the first 21 days. This is a time of rest for the new mother and the child. The mother-in-law moves into the room and takes on the responsibility to care for the newborn and the mother. The mother-in-law washes both her grandchild’s and daughter-in-law’s clothes so that the mother and child do not catch a cold. The mother-in-law also prepares food and feeds her daughter-in-law. Some respondents shared that in their community, they make a fire in the room where the mother and child are staying and warm up a cloth to wipe the baby. The mother also massages herself with oil during this period. The baby is given an oil massage twice a day, called bhumi shek, which involves pressing down the navel with a clean piece of cloth that is first pressed to a clean portion of the floor, which has been specially cleaned for this purpose during this period. The baby is given a bath with turmeric and warm water seven days after the initial period of confinement. Mothers are also restricted from taking a bath during their confinement. They are allowed to change clothes and wash hands and feet regularly. This 21-day period is an important period for the new mother as it gives her an opportunity to rest and be with her child. After this period, she is expected to go back to work, and her mother-in-law, with the help of other women in the household, takes care of the infant.
During the 21 days, our mothers-in-law sleep with us and the child in the same room. The mother-in-law does the work for the child. After 21 days, everybody can touch us.
-FGD with breastfeeding women
When the mother and child come back to the house, we (sassous) take care of them. They rest for nine days. The mother does not go out, and someone (mother-in-law, sister-in-law) stays with her. There is a fire in the room. We massage the child, and we warm the cloth by the fire. We put the cloth on the baby’s body so the baby’s body is warm. We warm up the child with the fire and massage with turmeric.
-FGD with mothers-in-law
3.1.4 Role of Husbands
Though husbands were not reported as playing such an active role in decision making regarding maternal and child health as the mothers-in-law, many pregnant and breastfeeding mothers reported confiding in their husbands when they were in conflict with their mother-in-law—for example, if they were still hungry and wanted to eat more or wanted a certain type of food that the mother-in-law was not approving. Thus, in many cases, the husbands were seen as the trusted member of the family, the last resource for the woman when/if in conflict with her mother-in-law. Many women reported that they could ask their husbands to buy some foods at the market if they needed something. In these situations, it seemed that the husband was the trusted partner, who ensured that his wife had what she wanted to eat. Some of them played a vital role by insisting that their wives took the IFA tablets and by ensuring that they were taken at the right time. Other husbands did not know about the importance of IFA. Regarding infant and young child feeding (IYCF), all of the four husbands interviewed reported very limited knowledge, and they felt that for their child to be healthy, it was better to give infant formula. One also reported that giving colostrum was not good for the child.
I really don’t know until what time my child should be breastfed. My wife had insufficient breast milk so immediately after birth we had to start Amul powdered milk as complementary food, and until now, we are continuing partly mother’s milk and partly Amul powdered milk. We did not give the colostrum. It was thrown out because we feel that the baby will not able to digest it and it will lead to loose motion of baby.
-IDI with father of children less than two years of age
My wife has never taken iron tablets during all the pregnancy times. I don’t know these tablets. I know that hot food should be served to the lactating mother after childbirth. Greens should be eaten. My wife had a lump in the breast so she could not give milk to baby in one breast.
-IDI with father of children less than two years of age
During pregnancy, my wife has taken all the iron tablets and other medicines as prescribed by the doctor. During her pregnancy, there were no restrictions on what she could eat...but after the child’s birth there is restriction of eating black eggplant and broiler chicken for six months, and fish for one month. My wife used to eat hot food till two to three months after childbirth.
-IDI with father of children less than two years of age
Within six months of childbirth, I gave gripe water to the child, and bonnison, and water apart from mother’s milk. My wife takes the decision on what the children will eat and whenever they go outside they carry some biscuits with them. No one in our village has ever given us some advice of what our children should eat. I am not sure what should be given to eat after six months...I don’t know. I believe they should be given everything to eat after six months, anything that is available within the house, but not sure when and what.
-IDI with father of children less than two years of age
After two months, we started formula food for the child as our relatives suggested us to do so. Our baby was weak so our relatives also suggested giving powders. Now our daughter is weak but I don’t have sufficient money to buy vitamins for her...My wife took a few iron tablets after I insisted; otherwise, she was not interested due to bad taste.
-IDI with father of children less than two years of age
All pregnant and lactating mothers interviewed were positive about the support they received from their husbands during the pregnancy. They shared that their husband tries to help them and also assures that they have access to the foods the women want to eat. Husbands were seen as trusted partners, although with limited influence regarding childrearing and maternal nutrition, as compared to mothers-in-law.
In our mother-in-law’s house, when we want to eat something we tell our husbands and they bring it from the market. If they bring the raw material in the morning, we cook and consume in the evening.
-FGD with pregnant women
My husband helps me if no one is there. He helps me in cooking and if I am ill, he helps me.
-IDI with pregnant woman
In addition to husbands, other family members, such as sisters-in-law, were reported as a source of advice and support.
I plan on only giving him my milk until he is six months old and then he will have rice and dhal. I don’t know how often to feed my child rice and dhal. I don’t know, but my sister-in-law will help me, she has children.
-IDI with mother with child less than six months old
3.2 Objective 2: Identify the Current MIYCN Practices and Barriers That Need to Be Addressed
3.2.1 Timely Initiation of Breastfeeding
Timely initiation of breastfeeding was found to be a common practice: most women (95 percent of lactating women) reported breastfeeding their child within one hour of birth. All women reported giving colostrum, although one man reported that his wife discarded the colostrum. Giving colostrum is now explained as being part of the traditions around birth. First, the new child is washed and massaged with turmeric, the mother is also cleaned, and then the baby is put to the breast. Many mothers reported that they knew they had to give the first milk, referred to as kasakheer. Most women reported giving the child colsotrum, but they did not know the importance of giving this first milk to the child, and it appears that this is not actually the decision of the mother, but rather something done by the birth attendant—the ASHA or mother-in-law. There is generally no prior explanation during pregnancy about the importance of feeding the newborn colostrum.
After the birth, definitely the child and mother are cleaned, then my child was put to my breast, I started breastfeeding within two minutes. I am not sure why I need to breastfeed immediately but I know I have to, I think it is required...It will keep the body warm for the child. It will give me stimulation for my breastfeeding. I know this by experience, after my first child. I give the first milk. It helps make the baby healthy; it always keeps the baby well. The child is well, everything goes well. I still only give breast milk. I know to give breast milk, when the child cries. I usually give breast milk every two or three hours. If the child cries, I immediately give her breast milk.
-IDI with mother with child less than six months old
After bathing the mother and child with turmeric powder and soap, I gave breast milk. After completing the bath, I gave my first milk—thin milk.
-IDI with mother with child less than six months old
When the baby was born, first they cleaned my child and me. Then they gave the baby to me to breastfeed. They keep it like this and I don’t know why...only feed the baby mother’s milk. I don’t know how often I feed my baby, I only breastfeed my baby, I don’t know how many times, but I breastfeed him whenever the baby is crying, I don’t count.
-IDI with mother with child less than six months old
3.2.2 Exclusive Breastfeeding up to Six Months
Although mothers and mothers-in-law reported that exclusive breastfeeding was the best food for the child, when probed, many of these same women reported that soon after birth, the newborn was introduced to other forms of foods and liquids, especially when neighbors came to visit, as this is part of tradition. Also, when the child is born during the hot season, there is a popular belief that the baby needs more water. If the baby is crying, this is seen as an indication for needing gripe water. Respondents widely shared that newborns and very young children were introduced to other liquids and foods early on. Several women reported being worried about the quantity of milk they were making and the inability to feed their children. A few reported thinking that their breast milk was causing the child to cry, because it was “bitter milk.” No woman reported knowing that a breastfeeding mother makes more milk as the child suckles.
Mothers breastfeed at first, and they give the colostrum. That is not the problem. Now women know to give the colostrum, but it is more about women giving other foods. Some women give honey, some women give water and sugar, and some women buy gripe water from the store. When the baby cries, they give the baby gripe water. Some women, in addition to the breast milk, give milk powder. They do both breast milk and milk powder. When the baby cries, the mother thinks the baby has not enough breast milk so she gives more food, she gives milk powder. Some mothers think they don’t make enough milk. Some mothers and caregivers (mothers-in-law) don’t know that the more the child breastfeeds the more milk the mother makes.
-KII with nutrition focal person of Panchayat
I am bottle feeding the baby from two months. No milk comes from my breast, from two months the milk decreased. My mother-in-law told me that I do not have sufficient milk. My mother-in-law advised me to start bottle feeding.
-FGD with breastfeeding mothers with children less than six months old
I think my milk is bitter, I don’t think my child likes my milk, I don’t think the child is drinking enough milk so I decided to give bottle feeding.
-FGD with breastfeeding mothers with children less than six months old
In addition, many respondents shared that although they knew about exclusive breastfeeding, they were not sure how often and how long the baby should be exclusively breastfed. Some mothers reported feeding the child when the child was crying; others reported feeding the child when the child was brought to them, while they are working in the field, as most women reported having to return to fieldwork after the first 21 days of rest. Many mothers reported leaving their child either in the home with an elderly caregiver (often the mother-in-law) or bringing the child to the field and leaving him/her by the edge of the field with a “minder.” Often, by the time the child is brought to them, the child is crying and hungry and has been soothed with biscuits. Some mothers reported introducing complementary foods around the fourth month, whereas mothers from some tribes reported that delaying introduction of complementary foods until after the ninth month was the tradition.
After 21 days, we can go back and work in the field. When I go to the field, I leave the child at home with the mother-in-law and the child is hungry until I come back home.
-FGD with mothers with child less than six months old
3.2.3 Continued Breastfeeding up to Two Years
Most mothers reported that they continue breastfeeding during the first two years, and some up to the third year.
The child will have the mother’s milk, what else will the child have? The small child will have the mother’s milk.
-FGD with mothers with children less than two years
A few breastfeeding mothers, although not giving formula, reported that they would prefer to give it. Many mothers reported that being able to give formula was associated with status and having enough money to feed one’s child well. Several women reported being influenced by their husband in choosing to introduce baby formula.
My husband gives importance to baby food for having a lovely child. My husband visits everywhere. He saw a picture of a healthy baby on the baby food packet. If my baby gets this food, my baby will be a lovely child, so my husband bought the food packet. I gave the food to the child, and I am also breastfeeding.
-FGD with mothers with children less than two years
3.2.4 Complementary Feeding
From the IDIs and FGDs with mothers-in-law, pregnant women, and breastfeeding mothers, it appears that families have very limited knowledge of when to introduce complementary foods. The practice varies from introduction of foods by the second month to past nine months. In addition, when asked what types of foods were first introduced to the child, all women reported “watery dhal and rice biscuits.” Based on these discussions, it appears that there are no special foods made for the child who is older than six months and less than two years old, other than the dhal that is usually eaten by the family, diluted for young children. There was no concept of introducing snacks and feeding the child more frequently than the meals consumed during the regular family mealtimes. All respondents shared that giving rice cakes to a crying child was common practice. Based on discussions with the UNICEF Regional Advisor and the ANMs, it appears that there is a critical need to focus on the appopriately timed introduction of complementary foods, as well as the consistency and frequency of feeds.
Complementary foods are critical to address; there is a lack of understanding of the need to diversify foods and there are so many inappropriate foods given, such as dhal kapani (watery dhal). Mothers are breastfeeding up to the fourth month in general, but they don’t know when to introduce complementary foods and what types to introduce.
-KII with UNICEF Regional Advisor, Keonjhar district
Introduction of Complementary Foods
Most women reported not being sure when to introduce complementary foods, and the practice varied across respondents. Some reported introducing “solids” (watery rice) by the second month, others by the fourth to fifth month, which seemed the most common practice. Many reported delaying the introduction of complementary foods until the seventh or eighth month. The common thread across all respondents was that women were unsure when to introduce new complementary foods and thus followed the advice of their mothers-in-law.
Before introducing any kind of food, I ask my mother-in-law what foods I can introduce. After eight months, I introduced foods. There was sufficient milk until eight months, and even now I still breastfeed.
-IDI with mother with child less than two years
My mother-in-law has told me to mix boiled rice with milk and sugar and give it to my child. This is good for my child. I give my child foods two to three times a day. I give it by myself. I don’t ask anybody. At seven months, my child started to have other foods than breast milk. I think I want to get Horlicks (a malt milk drink) for my child to make her strong.
-IDI with mother with child less than two years
Some families, in the scheduled tribes, don’t give foods to babies until the baby is one year old. Some families wait until the seventh month. This is tradition. In other families, members of the families eat the food given for the children from the Angwandi center. The child does not get the food, as the families are very poor and the adults eat the food.
-KII with ANM
Chatua and Other Foods Used as Complementary Foods
The GoI has put in place a scheme to provide food rations once a month to families below the poverty level. This food ration, known as chatua—a mixture of peas, green chickpeas, sugar, and peanuts—is calculated based on the number of family members and is targeted to pregnant women and children older than six months. There is often confusion, however, about when the chatua should be introduced to the child. Many respondents explained that the chatua is shared among family members, but also used as a complementary food. Some women explained that they give chatua only once a week to their child, while others give it daily.
We give chatua. We get two kilograms per month from the Anganwadi worker. We give it twice a day, two spoons mixed with water in the morning and in the evening. We increase the amount depending on what the child can take. We mix it with water or milk depending on what we have. We still continue with breast milk until three years old. In addition to this, we give kitchuri at noon, once a day. We mix vegetables, rice, dhal, papaya (cooked green papaya), potato, carrots, and beets. We mixd it and make kitchuri. We mix chura (flattened rice) with water and make rice cake and give in the morning and in the evening.
-FGD with mothers with children less than two years
I have introduced chatua after the seventh month. The chatua given by the Anganwadi worker gets finished in 15 days. I increase or decrease the quantity of chatua depending on what my child wants to eat. At eight o’clock in the morning, I give chatua to my child. Around 10 or 11 o’clock, I give Cerelac, and around two o’clock I give a regular lunch of rice, dhal, vegetables, or whatever is cooked for the family. At five o clock, I give another feed, and in-between I give breast milk. In the evening I give my child dinner—six to seven meals. I don’t give spicy food to my child. I give boiled foods to my child as spicy food will cause diarrhea. Sometimes instead of chatua, I give pita (the rice cake) and I make it soft by crumbling it to give to the child. Whenever I give rice with dhal to the child, I dilute it with liquid to make watery dhal.
-IDI with mother with child less than two years
Types of Foods, Consistency, and Frequency
Most women reported giving watery rice with dhal, sometimes giving only the cooking water of the dhal with salt. Many women reported giving chura—rice cake—as a morning and evening food. Mothers reported that they were aware of cold foods (foods associated with giving a child a cold) and hot foods. Fruits such as ripe bananas, papayas, mangos, and jackfruits were seen as cold foods and were not given to young children.
Children have their own food, and the food is on its own plate. There is no problem, the young child has its own bowl, but the problem is the food, it is very watery, mashed dhal, potato, rice, but not much dhal, very watery. The mother often mashes rice and potatoes, she also prepares rice cakes and that is what the child eats. Rice and potato, three or four times a day. But in very traditional families, most children eat only twice a day. Most women don’t give vegetables, only rice and potato or rice cake. Eggs are strictly prohibited. Eggs are not digestible. They are afraid their children will have diarrhea. No fish up to one year—the child cannot eat fish. The mother also does not eat fish for a year after she gives birth. Nobody takes ripe papaya, this is a cold food. We have many cold foods that cannot be given to the child or mother. If they eat cold foods, they will have a fever or a cold. For the first six month to a year, children only eat rice and dhal, after they start increasing other vegetables. Mothers continue to breast feed during two years.
-KII with Nutrition Focal Person of Panchayat
I plan to breastfeed for more than a year, not less than that. I plan on breastfeeding, it will continue and then I will give additional foods. This will start seven months onward. I will give rice, boiled potato, boiled papaya. We can give a little bit of eggs by the eighth or ninth month. We don’t give ripe papaya to the child, the baby will catch a cold. Dahl, rice, potato, and cooked papaya, that is what we know and that is what we give...I think the child needs to be fed three times when the child starts eating, that is what I think, three times a day.
-IDI with mother with child less than six months
After six months I gave some food, boiled vegetables, dhal water with small amount of rice to make it like a cream. I did not purchase packaged food, but I give papaya (cooked), eggplant, beans, and it is all mixed and mashed by hand. It’s hard to explain how much I give, a pinch full [she shows by holding her fingers together]. I give this six to seven times a day. At first, I often give her small quantities. Past one year, she can eat a little bit of egg, but I don’t give papaya not cooked or banana, because these foods give a cold to the baby. If we give some, we have to give in small quantities. My child eats everything. She even eats fish and chicken and sometimes liver and mutton.
-IDI with mother with child less than two years
Other Practices Related to Feeding
Feeding During Illness: Most, but not all mothers, reported continuing to breastfeed their children during illnesses. Many said that they stop giving all other foods, and reduce the amount of breast milk given, because they think that giving more food will lead to the child having more problems with digestion during the illness.
Mothers reported that it seems obvious to breastfeed the child when the child is ill, as this is a way to comfort the child. as most mothers continue to breastfeed for about two years, when the child is ill, they often see breastfeeding not only as a source of food but also as a source of comfort. When breastfeeding mothers are ill themselves, however, it appears that they stop breastfeeding, as they fear that the illness will come through the breast milk.
When the child is ill, the child prefers breast milk more than any other foods, but the amount reduces.
-IDI with mother with child less than two years
When she is ill, she likes to eat green leafy vegetables and soft rice, biscuits, and bread. If she has diarrhea, she likes rice and sagh (leaves).
-IDI with mother with child less than two years
When ill, mothers don’t go to the doctor, they prefer to go to the “quack.” Mothers stop breastfeeding when the child is sick. Mothers stop breastfeeding when they are sick as they think the illness goes with the milk.
-KII with nutrition focal person of Panchayat
Eating Out of Their Own Bowl and Hygiene
Children have an individual bowl, katori. If a bowl is not available, mothers reported using bowls made of banana leaves or putting the food on a leaf. Although very young children have a spoon, they are often fed by hand by the caregiver, and are soon encouraged to eat with their own hands. Although respondents explained that they knew that it was important to wash hands before eating, many reported that in their community “handwashing is a problem.”
Mothers reported knowing that to feed the child, they had to use clean water and would boil well water. However, although mothers reported cleaning their hands to prepare foods, or after defecation, when other key informants were interviewed, they highlighted the limited practice of handwashing as a key factor driving children’s diarrheal diseases in the community.
I have a separate bowl and spoon for my child. When I feed my child I don’t make it very thin or lumpy I just make it right. I don’t crush the food, I let the food be. (I don’t crush the rice.) I give water from the well but I boil it first. On average, I breastfeed my child five to six times a day.
-IDI with mother with child less than two years
3.3 Objective 3: Identify the Major Nutritional Issues Women Face, Including Societal Structures, Taboos, Barriers, and Promising Practices to Build Upon
3.3.1 Differences in Family Practices Due to Tribal Traditions and Socioeconomic Factors
It should be noted that this research was conducted in a small sample of rural villages in Keonjhar district, and thus the findings from this rapid assessment are reflective of the contextual realities of these villages in remote rural areas, with a predominance of ST inhabitants, a group of people who over centuries in India have been deprived of equitable access to education and health care. These findings are not specifically representative of India, but are representative of the contextual realities of the sampled villages. It is also important to understand that society is rapidly changing, as illustrated by the FGDs with pregnant women and other women who have had access to education. Despite the differences among tribes and within families, one recurring theme that came through strongly during the research was the limited agency of the pregnant women and breastfeeding mothers who live in the extended family context, where the mothers-in-law are still the major decision makers in the home.
Through this formative research, several factors affecting the lives of women and their children were identified. Families’ contextual realities vary within Keonjhar, due in part to the different tribal traditions, but also due to various other socioeconomic factors within individual families. Higher levels of education have been identified as a positive and protective factor for maternal and infant nutrition. In households where someone had attended school, respondents reported exclusively breastfeeding the child for the first six months and women reported facing fewer taboos. They also reported being well treated, eating enough, and having a chance to rest during the first six months of the life of the child.
The Munda (tribe) women have to work a lot, until they give birth and then they have to go back to work nine days after giving birth.
-FGD with mothers-in-law
In our community, there are a lot of women who give sugar, honey, and have pre-lacteal practices but for me, in my family, I am well taken care of because my family is well educated. My brothers have a good level of education and are working outside of the village. My father-in-law is a teacher, so he also knows what is good for the child and mother. All my family is making sure I can take care of myself.
-IDI with pregnant woman
Families are different—my family treats me well because of the level of education. It differs because of the level of education of family…My mother-in-law knows. Everyone in my family knows.
-IDI with mother of child less than two years old
3.3.2 Practices Are Changing: Fewer Food Taboos and Greater Understanding of the Need to Rest During Pregnancy and During the Postpartum Period
Change Might Not Be Happening Fast Enough for the Newer Generations
During the FGD with the mothers-in-law, the older women compared their lives during pregnancy and motherhood with the lives of their daughters-in-law, and reported that now, although there are still food restrictions, they are fewer in number, which generally don’t last more than six months, as compared to the one year that they had to endure.
You know, in our communities, some families restrict fish and chicken for daughters-in-law. There are still some food restrictions in limited families, but most people have started allowing them to eat foods, but there are still some restrictions. During our time, when we were pregnant, it was all restricted, but now it’s less. Before we had restrictions until the child was up to one year old. You should have seen how weak and tired the mothers were! But now, in most families, we don’t have these restrictions, but still some families have them.
-FGD with mothers-in-law
There are no traditional practices preventing the woman to eat anything during pregnancy. After the child is born, burnt things are given to the new mother. We give more of eggplant and garlic. We don’t give spicy food, sour foods, poi, and lady finger is not given. Earlier, when a child was born, mothers were given food and water only once, now the mother is given food three times a day.
-FGD Panchayat leaders
Greater Understanding of the Need to Rest during Pregnancy
The mothers-in-law reported that there is a better understanding of the need for pregnant women and breastfeeding mothers to rest: “This is a must for the child and women to remain healthy.” Mothers-in-law reported that, during pregnancy, to help their pregnant daughters-in-law, they themselves take on some of the daughter-in-law’s tasks, mostly the outside activities such as fetching water and cleaning the shed. After delivery, the new mother is expected to rest for the first 21 days, and the mother-in-law moves into her room to help with the child.
It was the practice for us to work until we deliver. It was to make us strong. But now it has been changed. Pregnant women should take rest—two hours a day, they should take rest…Sometimes we divide the work, we share the work with our daughters-in-law, and we give them relaxation. Our daughters-in-law share the work with us. We divide inside the house, the daughter-in-law after giving birth stays inside the house and does inside work, and we do the outside work. We clean the cow shed, we fetch water. Our daughter-in-law does the cooking, and serving of foods and clearing. Outdoor work we do. Rest is a must, but after lunch. She must take rest after lunch, even if someone comes to the house, then the mother-in-law must take care of the guests, she cannot be disturbed.
-FGD with mothers-in-law
However, it is interesting to note that during the FGD with pregnant women and breastfeeding mothers, many reported that they still faced a heavy workload during their pregnancy, such as fetching water and wood, cooking and serving meals, and cleaning the outside courtyard and cow shed. Many women described their daily tasks and the family expectations for them to continue to work until delivery, from a belief that this would make them strong.
Many mothers-in-law recommend us to work hard, so that the delivery will be easier. There is a chance of early delivery, sometimes the pain continues for a long time, so the pain period will be less if the pregnant woman works hard during pregnancy.
-FGD with pregnant women
One change that seems to be almost universal is that during the harvesting season, most pregnant women don’t go to the field in their last months of pregnancy, and don’t return to the field after the first month of giving birth (the first 21 days after birth). As illustrated by the discussions with the mothers-in-law and younger women, the concept of rest is understood, but the realities of workload put many demands on the pregnant woman and new mother. It is important to highlight that in many cases, the workload shifts to more fieldwork taken on by the mother-in-law or other sisters-in-law, husbands, or even parents of the woman, and the housework remains with the pregnant woman or new mother.
In terms of work, I have a lot of work. I clean the cow shed, the courtyard needs to be done with cow dung. My husband gives me some support by providing some help, but now everything is going on, this is the time of the harvest for the paddy...So my parents come to help my husband. My mother-in-law cannot help. I have a lot of housework. Three or four times a day I sweep the courtyard, I need to wash the house inside daily. Before being pregnant I was helping my husband with the paddy, but now I am not helping, I am working in the home. I go to the field to bring food to my husband.
-IDI with pregnant woman
Families as Supportive Entities
All women reported that within the families, there are a lot of supportive systems, where women share work, including responsibilities for caring for the new mother during the first 21 days after birth, and for the young child when the mother needs return to the field to work. Women are not isolated, as they have a built-in support system within their families, which includes mothers-in-law, sisters-in-law, and husbands when they return from fieldwork.
The First 21 Days Postpartum
After giving birth, the mother and newborn stay in one room, and the mother-in-law moves into this room to help care for both the new mother and baby. She is the primary contact with the outside world, as the new mother is not supposed to go out, and is not supposed to be touched by others. During this period, the mother-in-law decides what the new mother can eat, prepares her food, massages the new mother and newborn, and also decides, in most cases, if the child will be given gripe water, water, and/or honey. During this period, the mother-in-law is continuously there, providing advice and caring for the new mother and child.
After giving birth, I don’t go anywhere for 21 days, I have to stay inside the house. I don’t do any work for one month, I take rest. During the one-month period, I stay inside the house, maybe I do some small housework, but I do not do much for the first month. I rest. I have my mother-in-law and she takes care of the baby with me.
-IDI with mother
Going Back to Work and Childcare Practices
All women interviewed reported that after the first 21 days of rest, they had to get back to work, and “shoulder their responsibilities.” Childcare practices seem to differ greatly. Some mothers reported taking the child with them to the field while others reported leaving the child in the care of the mother-in-law. Mothers reported that the mother-in-law is in charge of taking care of the very young child, and if the child “cries too much” the child is brought to her when she is working in the field. The common thread of all these stories is that women after the first 21 days have to go back to work in the paddies (rice field). Many women reported being tired from having to go back to the field work right away, but really have no choice because the family needs their help.
We would like to look after our children and we think of their welfare, but our mother-in-law gives us a lot of work, then we are not able to take care of the children. We don’t have the time.
-FGD with mothers with children less than six months
3.3.3 Maternal Nutritional Practices During Pregnancy and Breastfeeding Period
Enabling Factors
Good Understanding of the Need to Eat High-Quality Foods: Most women reported knowing that they “have to eat a balanced diet,” with different foods, but actually they shared that during their pregnancy, they eat the same food as the family eats, because the household lacks the income to buy diverse, higher-quality foods.
I know that I should eat eggs, milk, and fruits. Our in-laws suggest that we eat this, but it’s very difficult to afford. Whatever the family eats, I eat. I eat the same food as the family.
-FGD with pregnant women
Although there is a high awareness of the need to eat vegetables, eggs, fish, meat, and pulses, most women reported eating only dhal and rice, as this is what the family is able to purchase. Many pregnant women (80 percent) reported that their mothers-in-law believe that during pregnancy women should eat less to avoid having the fetus growing too big, which would lead to complications during delivery. However, as described above, some beliefs and traditions are changing. Many younger pregnant women and breastfeeding mothers reported that although their mothers-in-law advise them about the type of foods to eat and the quantity, these younger women also receive advice from the ANM and ASHA and are therefore becoming more empowered to make their own, informed choices.
Our mothers-in-law suggest to eat less so that the baby will not grow so big...We believe we should eat less times but more quantity, when we are hungry. But our mothers-in-law suggest to eat less...but that does not happen, we feel hungry and so we eat as much as we want. Now we eat more times and more food.
-FGD with pregnant women
Other pregnant women reported knowing that “good food is necessary during pregnancy,” but were unclear for which reasons and stated that food would help them to deal with the pains of giving birth and also would ensure that their newborn was healthy. Although the information might be limited, most pregnant women could explain that eating higher-quality foods during pregnancy would help them and their child.
Good food is required. It lessens the pains when we give birth. I will have the stamina to give birth and I will have the stamina to register for the pains. There might be many other things that I don’t know much, but I think the child will be in good health also.
-IDI with pregnant women
Barriers Affecting Optimal Maternal Nutrition
Gender Role within the Family: Pregnant women also reported instances of “going to bed hungry” once or twice a week, especially if there were guests, or if food ran short. Almost all of them ate only after they had fed the other family members, including their children, husbands, mother- and father-in-laws, brother- and sister-in-laws. The women also reported that mealtimes were likely to change based on the amount of housework. The first meal of the day was reported at 10 or 11 AM, while the next meal was around 4 or 5 PM. Pregnant women started their day at around 5–5:30 AM.
Food Taboos: Food taboos were reported mostly during the postpartum care period, for the first six months of life of the new child. As mentioned previously, the food taboos are changing as mothers-in-law reported that “during their time, there were food taboos until the child walked, for the first year of the child.” Many of the food taboos are linked to the quantity of foods a breastfeeding mother can consume. Many breastfeeding mothers reported that their mothers-in-law advised them not to eat too much, because if they did, the newborn child would face an increasing risk of not being able to digest the breast milk. In most communities, women reported eating only rice, kulthi dhal, and burnt brinjal (eggplant) during the first 21-day period. Most women reported having only two meals a day, while some reported eating only once a day. Drinking water was also restricted to the same number of times.
My mother-in-law said that the mother should take rice twice per day for up to three months after giving birth, and after three months she should take rice more than three times. At the beginning, she needs to take two meals a day…My mother-in-law told me to take two meals a day because the baby eats small amounts, the baby is small, when the baby grows a bit more, then my mother-in-law said I can eat more times, three times a day.
-FGD with pregnant women
Up to 21 days, we are given garlic, boiled eggplant, khulti dhal, mashed potato to eat, and that’s it. We have meals at two times, once at 10 AM and once around 21 to 22 hours in the evening. Our in-laws have asked us to stop eating more times because the child will not be able to digest…During this period, I can only drink water twice a day. We don’t have biscuits or any other thing. We feel tired and weak.
-FGD with breastfeeding women
My mother-in-law tells me the child will get sick if I eat different foods. If I eat more, the mother cannot digest the food and the child will have digestive problems. I believe my mother-in-law. I won’t be able to digest the food, I believe my mother-in-law, she knows. I will tell my children this later when I am a mother-in-law. I eat different foods than the rest of the family. I can only eat boiled rice, pumpkin, potatoes, but I am not feeling hungry, I am okay. I am not sure how long I will have to eat these different foods. My mother-in-law did not tell me yet, so I don’t know. Everyone else in my family is eating different foods, some kind of spinach, sometimes also chicken, sometimes eggs also, but me, I eat different foods and I don’t know for how long.
-IDI with mother with child less than six months
There are other taboo foods, with many classified as hot or cold foods (which may be based on or attributed to ayurvedic principles). These taboos are quite specific to the different tribes and families. Some foods are believed to help the breastfeeding mother produce more milk, such as the bitter gourd and brinjal (eggplant); other foods are believed to be “cold foods,” such as ripe papaya and pineapple, which if consumed by the mother, will cause the child to become sick. Some foods, such as eggs, are totally prohibited by some tribes. Since the taboos vary according to tribe, clearly understanding the contextual realities of the villages is necessary.
After we give birth, there are foods we cannot eat. There are some restrictions. We cannot eat black dhal seed, lady finger, pumpkin, peas. There are also two varieties of drumsticks. We can eat one variety but the other kind we are not allowed to eat. We eat cooked papaya but not ripe papaya. We can eat mango when mangos are in season, but it depends on the season. I don’t eat fruits every day, maybe once every four days, when we go to the market.
-IDI with pregnant woman
My mother-in-law told me as a mother, I should take bitter gourd, brinjal, and dhal when I give milk to my child. These vegetables help the mother produce a lot of milk, and it is easy for digestion for mothers so she gives me this bitter gourd because the mother will have sufficient milk.
-FGD with breastfeeding women
During this first month, I have to eat different foods. I have to eat different foods until the baby can crawl. I can only eat boiled food, dhal ground, hot rice, bitter gourd, garlic. All the food is boiled with water and this is all I can eat. I can only eat everything when the baby starts to crawl, but not before. My mother-in-law tells me that I cannot eat other foods, because if I eat them the body of the baby will get hot, the baby will have a fever.
-IDI with mother with child less than six months
During the first month, I can only eat twice a day, once in the morning and once in the evening. After the first month, I can eat three times a day, but not before. The first month I can eat only twice a day. At first, I feel hungry, but it becomes a practice. There is a ritual, this is part of my family, it takes three to five days to get used to the food and being hungry, it takes some days to settle, but even if we are hungry we cannot do anything. This is what is decided by the elders. [What does your husband think?] He goes by his mother, this is a family tradition. After the baby crawls, there will be no restrictions, and I will eat like the whole family.
-IDI with mother with child less than six months
IFA Supplementation: Most mothers are aware of the “tablets” given during antenatal care (ANC). When asked, women could not really give specific information about anemia, “the thin blood disease,” but they knew that IFA was supposed to “make them strong” for the delivery of their child. Women had very limited information about the tablets; they were unable to clearly state in which month of pregnancy they were expected to start consuming these tablets and how long they should continue. The quantity of tablets to be taken was not consistent, and it appears that the ANMs and ASHAs are not clear on the GoI protocol, with quantities varying from giving 30 tablets once to giving 200 tablets if a woman shows signs of anemia (through a hemoglobin test). All pregnant women reported limited counseling on how best to take the tablets and cope with side effects. It is important to note that the consumption of IFA varies according to the understanding of pregnant women. Some reported taking the IFA regardless of side effects as they knew this was good for the future child, while others reported taking only two tablets, because they were unable to cope with the side effects and had received limited counseling about them. In addition, it is important to highlight, again, that as times are changing, more women are receiving advice about IFA from the ASHAs and ANMs, and although mothers-in-law have reported not trusting the IFA tablets because they might make the delivery painful, more women reported listening to the ASHAs and ANMs.
…but whenever we collect the tablets, they never tell us the benefits of these tablets, they just tell us to take them. Just take these tablets. In case of any problem you contact the ASHA. We don’t feel bad taking these tablets... we are eating for the sake of our child.
-FGD with pregnant women
I only had one month (30 pills) during my fifth month of pregnancy. I started vomiting when I got the tablets so I stopped taking them. I was taking them in the morning, after breakfast. I stopped taking them. Nobody told me to keep taking them or stop taking them. I stopped because I was vomiting. The AWW gave me the IFA (30), and she told me to take them either in the morning or evening, she told me your child will be healthy and the mother will be healthy. She did not tell me anything else. When the ASHA comes, she asks if I take the tablets. I told her I was vomiting. She did not ask for more. I think I have three or four tablets left at home. I am not sure.
-IDI with mother with child less than six months
Everybody takes IFA, some mothers-in-law ask some pregnant women not to take the IFA because the baby will grow big and this will create problems during delivery. But the ANM tells us to continue taking all the tablets.
-FGD with pregnant women
3.4 Objective 4: Understand the Current Hygiene Practice with a Focus on Handwashing with Soap
This formative research tried to identify what the current practices are regarding handwashing, and the barriers to adopting this behavior. It was reported (and observed) in the study villages that there is generally wide availability of water from two sources—the village pumps and the water well. Households reported that water collected from the well is boiled to prepare food with, but during interviews with Panchayat leaders, they reported that, in fact, the practice of not boiling drinking water obtained from the wells is a major reason for the high level of diarrheal diseases in their villages.
It is within the Indian traditions to wash hands before eating or feeding a child, though most of the handwashing is done by rinsing with or dipping the right hand into a bit of clear water, usually with no soap. Usually, as observed during the research, a pot of water is standing next to the area where meals are prepared and eaten. However, during KIIs, all respondents shared that washing hands with soap is not a common practice. The Anganwadi center walls often depict pictorial messages about how best to store clean water, and the importance of handwashing. The AWW who was interviewed shared that during home visits, she talks about the importance of handwashing. During observation visits at the Anganwadi center (AWC), researchers observed that very young children, less than three years old, had their hands rinsed with water, but no soap, before eating. The AWW just poured a bit of water over the right hand of the children and rubbed their hand with hers. She reported that handwashing is part of their teaching and that this is taking place during the visits at the AWC and during Mama Diwas days, where mothers are sensitized about how best to care for young children.
Open defecation rather than using a latrine was also described as a common practice, and the Panchayat leaders reported that latrines are used in times of “loose motion” but not during regular times. Panchayat Leaders and AWWs reported that there are many schemes to encourage households to use latrines, such as giving them a cash contribution toward the building of a latrine, but there is traditional resistance to building and using latrines.
After activities of the Village Health and Nutrition Day have started, people are repeatedly told about handwashing. Members are unable to check whether people are actually practicing handwashing. Women tend to wash hands before cooking and cutting vegetables. However, we cannot ensure handwashing after defecation. Usually people tend to wash hands with mud and ash after defecation but one cannot be sure that they all do, especially children. Some NGOs had constructed toilets, but they were small and incomplete. People do not use them. There are no toilets at present and there is open defaecation.
-KII with AWW
The majority of households have a toilet but it’s not used daily. They use toilets at night and they use latrines when they have loose motion. In other days, except rainy season, they go outside. They prefer to go outside. In the latrine, they have to carry a bucket of water. They prefer to go outside in the field.
-FGD with Panchayat leaders
They know about handwashing but not all about soap. Mothers who are cooking are using detergent for cleaning hands before going to the kitchen. Simply rub with soap and washed by water.
-FGD with Nutrition Committee members
In the village, educated mothers wash their hands and the hands of the kids before preparing foods and eating. Others don’t. Those belonging to the Munda hamlet, even if they are explained they don’t understand, they don’t do this (wash their hands). Handwashing after defecation is common among educated. Earlier they used to wash with ash, now they wash with soap.
-FGD with Panchayat leader
3.5 Objective 5: Identify Sources of Information Currently Used by Pregnant Women, Breastfeeding Mothers, and Also How Current Services and Providers Are Perceived
3.5.1 Increased Importance of Community Health Workers: ANMs, ASHAS, and AWW
The GoI has made considerable efforts into developing a community health system, where ASHAs focus on family planning and antenatal/postnatal care; link to a health center; and visit households where pregnant women and newborn children live. The ASHAs are expected to visit the family on a monthly basis and accompany the pregnant women to the health center for delivery. In addition to the ASHA, the ANM is the professional health worker, who conducts the four prenatal visits that are part of focused antental care (ANC). The ANM is usually the professional who assists the woman during delivery.
When the child is born, the AWW is the community health professional, usually a volunteer, who provides a food ration (chatua) on a monthly basis, and also organizes the early childhood development program at the AWC for children three to six years old. When enrolled, children receive a daily meal through the Integrated Childhood Development Services (ICDS). Thus, the AWW is seen as the key community professional who gives nutritional advice and supplemental food for very young children under six years of age, as well as pregnant women.
Most women during the interviews reported having been in contact with the ASHAs, AWWs, and ANMs, and said that these workers are a source of advice and care. As described above, the advice received from the professional health workers is seen as contributing to the changes of practice within families.
3.5.2 Increased Influence of the ANM and ASHAS and Greater Access to Maternal Health Services
Ninety percent of pregnant women interviewed reported having attended at least one ANC visit, defined as a visit with the ANM at the health center. During the ANC visit, women reported receiving their first tetanus toxoid (TT) injection and “tablets” (or IFA). Although respondents were unable to articulate the details of a checkup, they reported that they had attended some checkup sessions with the ANM. Many pregnant women were unable to explain when they needed to return for the next visit, but said that the ASHAs would be reminding them about the appointment time.
Pregnant and breastfeeding mothers reported a preference for delivering in a health center, which can be attributed to one of the social schemes implemented by the GoI, where pregnant women and ASHAs both receive a cash incentive for choosing to deliver at a health center. Under the Janani Suraksha Yojana (JSY) scheme, a sum of INR 1,400 is given to pregnant women to incentivize them to deliver at a facility. Some of the money is spent on transport, and some is spent on paying the ASHA to accompany them to ensure a quicker service. Some women reported listening to the ANM’s advice and preferring delivering in a facility as they knew that this ensures greater safety during delivery for herself and the newborn. There was also a greater understanding that, when delivering in the facility, new mothers can stay 48 hours and avoid having to return to work right away. It was found that home deliveries in the community had occurred only in cases of preterm birth, birth complications, or during the third or fourth birth (and so on). More than 80 percent of breastfeeding mothers had either delivered in a health facility or were planning to do so. In addition to these mothers’ increased awareness and education regarding the advantages and incentives for delivering at the health facility, the AWW and ASHA’s constant advice on this was a contributing factor.
In comparison to the past, today more babies are born in the hospital. All mothers use the Janani Express. The first- and second-born children are born in the medical center. The third and fourth child are born in the house.
-IDI with AWW
3.5.3 Incentives to Deliver at Health Facilities
Pregnant women receive funds if they choose to deliver at health facilities. During the interviews, pregnant women reported that they planned on using part of the funds to take the ASHAs with them to help facilitate having access to services; part of the funds would be used to pay for transport. There is more of an understanding of the importance for women to deliver at facilities; some of this can be attributed to the advice given by the ANM and ASHAs and also to the financial incentives given to pregnant women to deliver at facilities.
All women deliver at hospital. The ASHA takes the patient either in the Janani Express, which she can call on the phone, or else they take women to the hospital in autos. If an auto is used, out of 400 rupees, 300 is taken by the auto driver and 100 by the ASHA. We are getting lots of benefits from schemes like the janani suraksha yojana. The medical center at Ghatagaon is very clean, and there are good doctors.
-FGD with Panchayat leaders
3.5.4 Increased Role of Anganwadi Workers
During the discussions, it was clear that AWWs are perceived quite differently, depending on the community and the character and experience of the AWWs. Some have been reported as sharing expertise on how to feed the child, and in helping monitoring his/her development, while others are not trusted at all and are being accused of siphoning off some of the food supplementation for themselves. During the interviews, some community leaders vehemently shared their anger about the mispercepton that they misappropriate the food rations. Therefore, although the AWW is a potentially powerful vehicle for promoting women and child nutrition, depending on the individual, there is either tremendous trust and respect for this community agent or there is anger and mistrust.
The chatua we provide is not sufficient or of good quality. The quality of rice and wheat given through the AWC was of good quality. The chatua given at present is not of very good quality.
-FGD with AWWs
AWWs reported having a lot to do and thus having difficulties in meeting community needs. They are expected to lead early childhood development activities in the morning and provide a meal for each child under six years old, every day, 300 days per year. In addition, every two weeks they are expected to deliver a dry ration of food to families below the poverty line. The AWWs reported not receiving the money on time to buy the food ration and thus having difficulties meeting the delivery schedule.
AWWs have a lot of work. We give TT injections and IFA tablets to pregnant women, run a preschool, and make house visits. During house visits, we find out why children have not attended school, counsel mothers about food for mothers and children, importance of taking IFA tablets. We buy the dry rations ourselves and provide cooked food to the children attending the AWC. Earlier, self-help groups were running the center. However, it stopped, as it was difficult to meet the expenses. We do not get money for dry rations at the right time. Mothers are more interested in actual benefits (money and chatua) than to listening to what we have to say.
-FGD with AWWs
3.5.5 Organized Community-Level Structures
The GoI has instituted several policies and safety-net programs to help meet the health needs of its citizens. Respondents shared that there are lots of schemes in their communities, such as receiving INR 9,000 to build a latrine; receiving insecticide-treated nets; regular food ratios (chatua) for pregnant women and young children under three years old; school meals for children under six years old enrolled in the Early Childhood Development Services (ECDS) conducted in the AWCs; and school meals for primary school children attending school. In addition, during interviews, the Panchayat leaders reported having several outreach programs to raise the awareness of mothers regarding optimal childcare practices, including the Mama Diwas (once a month), where mothers and children receive messages about immunization, prevention of illnesses, sanitation and hygiene; and the monthly visit by women to the AWCs, where mothers, in addition to receiving the food ration, have their child’s growth monitored and where young children are immunized. (The researchers observed such a day, and although all children were weighed and measured, there was no discussion or counseling with the mothers).
Despite the efforts, the Panchayats shared that their communities face a high burden of disease related to poor hygiene, sanitation, and nutrition, as well as weakness in service delivery at the AWCs. Many respondents shared that in times of illnesses, their first line of response is to seek out the traditional village doctor, called a “quack,” rather than going to the health center, reporting more trust in the “quack” and also fearing the cost of medicines prescribed by health workers at health centers.
The Anganwadi Center and AWWs are not doing their work. The center is not clean. Mothers don’t take their children there. So the children are not immunized. Women and children are supposed to receive foods, dry foods and cooked food daily, but they don’t. Children don’t come, the distance is too far. Activities are not conducted. The AWWs are supposed to play, sing, play games, but this is not happening...Health education, cleanliness is not happening. This is all due to the negligence of the worker.
-KII with Panchayat leader
At the illness of children, they give first preference to go to the village quack, and if he suggests to the patient to take medicines, then they take the medicines. If the village quack fails, then they go to the health center, but first they go to the village quack. If this fails, the village quack tells them to go to the hospital. We are not getting any medicine free from the hospital. Whenever the doctor comes and visits the village, we get free medicine. We buy medicine when we go to hospital. There is no free medicine at the hospital.
-FGD with pregnant women
All mothers do not come for immunization. They are afraid of the fever the child gets. We give vitamin A at the center itself. In meetings with mothers, we have clearly said that mothers who do not bring their children for immunization will not be given 5,500 rupees under MAMATA scheme. AWW identifies the malnourished children and refers them to the higher authorities. We have also advised mothers of such children about providing more food and more nutritious food to them. We identify children by registering them, weighing them, measuring arm circumference.
-IDI with AWW
3.6 Objective 6: Identify the Perceptions of Community Members and Also Video Production and Dissemination Teams Regarding the Digital Green Videos
During the research, IDIs and an FGD were conducted with key informants of VARRAT’s video production team, also known as community resource persons (CRPs), and VARRAT’s community service providers (CSPs). The CSPs were especially targeted because they facilitate the weekly dissemination of videos through self-help groups (SHGs) at the community level. Several major themes were identified through these discussions.
According to the CRPs and CSPs, demonstration videos related to agriculture are better received by the community than testimonials. Engaging viewers in learning new techniques by watching how these are done is much more effective in getting people thinking about change. Also, CSPs suggested that demonstration videos would be much more versatile and could be shown not only with the SHGs, which is the regular targeted audience for the agricultural videos, but also through the existing community-based health systems: the Mamata Diwas and the Nutrition Days.2 Both the video production team and CSPs recommended a high involvement of the AWWs to help define the messages, to help during production, and to be included in some dissemination activities. Respondents recommended that the content of the key messages be reviewed by ASHAS and AWWs to ensure that these messages are correct and feasible within their communities.
Through demonstrations, and explaining while doing, farmers learn. They like to see what is happening. Farmers learn by seeing things as they are being explained.
-KII with video production team, VARRAT
Demonstrations are more powerful than testimonials, because once the videos are made, the videos can be shared during Mamata Diwas. This would help. We can shoot the videos, and then we can make serial stories with pregnant women and get help from the AWWs.
-FGD with CSPs, VARRAT
We will get the support from the AWWs and ASHAs to review the content of the video. We can set up a review committee.
-KII with video production team, VARRAT
During these discussions, both groups reported the need to be “sensitized” when showing how to breastfeed a child. Most respondents reported that use of an illustration or image might be better received at the community level than showing a mother actually breastfeeding. Although the groups reported that exclusive breastfeeding up to six months is not practiced, they did report that early initiation of breastfeeding within one hour was universal and that mothers-in-law were there to help the new mothers when they started breastfeeding, thus passing the expertise from generation to generation. The respondents listed many areas where nutrition-related videos needed to be made, especially around exclusive breastfeeding up to six months. The respondents shared that it is common practice to give “rice cake, gripe water, and honey” to the child after the first few weeks, and especially when the mother goes back to work, after the first 21 days. Videos on complementary feeding were also recommended, with a focus on consistency, since in most cases young children received “watery rice and watery dhal” and without any routine. Also, videos on hygiene, specifically washing hands, and child health, such as immunization, were needed. Respondents shared that specific videos might be made for viewing by the mothers-in-law and husbands, who needed to be scheduled separately.
The mother-in-law and pregnant women can watch in one place, but the fathers will have to be treated separately for some of the issues. Then we can have a debate on these issues.
-FGD with CSPs, VARRAT
A real problem is that they don’t go for immunization. The ASHAs don’t bring the children and the mothers don’t remember. They don’t know when to bring the child for immunization. Mothers also don’t listen to the ASHAs for immunization…We should make videos about the quantity and number of times children should be fed. Mothers and caregivers don’t know when to feed children and how often children need to eat.
-KII with health focal person, VARRAT
4. Discussion of Key Findings
4.1 Range of Factors That Influence Optimal MIYCN Practices
As identified by this formative research, many factors affect optimal MIYCN practices in Keonjhar district. Many are related to sociocultural and economic factors, such as the level of education within the households, where higher level of education in the family is associated with better MIYCN practices. Also, traditional gender-related social norms affect MIYCN practices, where many women have limited agency to decide when to eat, how much to eat or when to rest. Specific tribal traditions that require a woman to work beginning at nine days after giving birth, or require delaying the introduction of complementary foods until after the ninth month, or require “welcoming” the child by introducing honey, gripe water, or water within the first days of birth completely contradict evidence-based MICYN best practices. Family organizational structures, which are sometimes a great support for pregnant women and breastfeeding mothers, can also create confusion, especially when a mother-in-law’s advice contradicts that of the ASHAs and ANM. Economic status and household livelihoods often dictate what types of foods are consumed within the household, and influence when women can rest during their pregnancy and after the birth of their child. Often women need to go back to work in the fields at the end of 21 days after giving birth, leaving their children in the care of others in the home. These social, cultural, and economic realities underscore the fact that improving MIYCN practices goes far beyond increasing knowledge. Respondents shared, for example, that although they knew what to eat, or knew they had to rest, they did not always have the economic means to do so. The range of these sociocultural factors has serious implications for the SPRING/Digital Green pilot, since increasing the knowledge of pregnant and postpartum women on key MIYCN practices will not be enough. Other family members will need to be purposefully engaged and motivated, and external barriers may need to be simultaneously addressed to create an enabling environment in order to achieve the levels of behavior change that are needed.
Although lack of knowledge of MIYCN optimal practices is not the clear driver behind current MIYCN practices, this research indicates that there are areas where knowledge, information sharing, and skills need to be strengthened. Although timely initiation of breastfeeding within the first hour of birth is nearly universal, exclusive breastfeeding for the first six months of life is not. Most respondents shared that other foods (rice biscuits or chatua) and liquids are introduced on average by the fourth month of life of the child. Mothers reported not really knowing that breast milk provided enough liquid to the baby to prevent dehydration during the summer months. Complementary feeding was another area where respondents shared very limited knowledge about and understanding of what the child needs to eat over the next 18 months of his or her life. A lack of information about the timely introduction, frequency, quantity, and consistency were shared by all respondents, women and men alike.
It is important to reiterate that there are many traditional practices and food taboos that dictate what women can eat while they are breastfeeding, specifically for the first six months of the life of the child. Food taboos are very much embedded in culture and often are key factors that bind cultural groups together, keeping traditions alive. Although one might say that many taboos result from a lack of knowledge, they are nonetheless deeply embedded, and the mothers-in-law, although perhaps open to change, are very much the “keepers of these taboos.” It will be important for the program to identify which taboos are actually harmful and which ones are essentially harmless or neutral. Many taboos are grounded in the likelihood that these foods might create a stomachache for the child—thus spicy foods are discouraged, for example. In reality, this type of taboo is harmless and might, in fact, be a sound advice. What is key to understand further is how best to ensure that breastfeeding mothers have enough food to eat while breastfeeding, and have access to a healthy diversity of foods.
Another area of importance for prioritizing nutrition video content is the strongly held belief that IFA supplements, if taken during pregnancy, lead to bigger babies, with negative consequences. With high rates of anemia in India, this is a key misconception to address. It is more complex, however, than just raising the understanding of the pregnant women and mothers-in-law about the importance of IFA for a healthy delivery and a healthy child. Systemic supply issues may also need to be simultaneously addressed. It would not help to raise the awareness of women regarding IFA if it is not actually available in the community and/or routinely prescribed at health centers by the ANMs. The research findings highlighted that there is no consistent approach or platform for IFA supplementation during pregnancy in Keonjhar, and women often lack access to the supplements and/or receive very poor counseling about the importance of IFA and how to counteract common side effects.
Other factors that emerged during this formative research help to explain why current MIYCN practices are often related to larger systemic issues, which go beyond the scope of the SPRING/Digital Green collaboration. The research findings illustrate, for example, that although the AWW is critical in supporting optimal nutrition for women and children, in some cases she is trusted by the community, but in others she is not. Some AWWs are perceived as using some of the government schemes for their own benefit. Although the GoI has put in place many important schemes at community level, such as the Mama Diwas, depending on how the discussions are organized and managed, some of these have limited influence. The researchers, for example, observed a growth-monitoring session where children were weighed, weights were recorded, but no counseling of mothers took place. The ASHAs can be a reliable source of information but only if they provide outreach services. Many respondents shared that the ASHAs don’t come to their homes, contributing to a limited trust in some of the related government’s schemes. However, addressing these issues is far beyond the scope of this SPRING/Digital Green collaboration.
4.2 Behaviors That Seem “Ripe for Change”
It is important for SPRING/Digital Green to identify which behaviors are more “ripe for change,” with serious reflection on which practices can actually be changed, promoted, and/or supported within the context, established scope, and resources of this one-year project. Below is a summary of the key MIYCN-related practices or behaviors that—based on this research—seem most appropriate to focus on under the current project’s mandate to test the feasibility of introducing nutrition messages via human mediated technology on an ongoing agricultural platform. These key behaviors include decreasing women’s workload during pregnancy and breastfeeding; strengthening support for mother/child pairs following the first 21 days; promoting regular intake of IFA and iron-rich foods during pregnancy and postpartum (addressing the fear of having too big of a baby); promoting the health of breastfeeding mothers; complementary feeding; enriching complementary foods with locally grown foods; strengthening the role of husbands as supportive partners; enhancing the role of mothers-in-law in childcare practices; exclusive breastfeeding during the first six months of life; and handwashing with soap.
4.2.1 Decreasing Women’s Workload During Pregnancy and Breastfeeding
Many women and mothers-in-law responded that they know that women need to decrease their heavy workloads, and need to get more rest more during pregnancy and the early months of breastfeeding. They stated that they were open to change, as they realized themselves that times were changing. As the research highlighted, mothers-in-law are cognizant that pregnant women and breastfeeding mothers seem healthier than they were themselves when starting a family. Many mothers-in-law shared that they are definitely aware of the need for their daughters-in-law to rest, and many are trying to support them by shifting some of the workload, especially heavy fieldwork, to themselves. Pregnant women reported knowing that they need to rest during pregnancy but at times felt that they could not, due to their responsibilities within the home and family. Engaging with mothers-in-law, building on positive examples of mothers-in-law who take on more responsibilities so that their pregnant and breastfeeding daughters-in-law can rest, sharing “role models” of mothers-in-law who have promoted task shifting within the homes, might be a viable strategy to promote positive changes in these work-related behaviors.
4.2.2 Strengthening Support for Mother/Child Pairs Following the First 21 Days
Many women reported having to go back to work after the 21 days of confinement, and most of them reported having to go back to work outside in the fields. Others reported that although they had to go back to work, they could either work at home, on house or compound work–related jobs (cleaning the cow shed, cooking, sweeping the courtyard), or go to the fields with a dedicated “childcare provider”—usually an elder women who kept an eye on the child and brought the child to the mother when the child was crying. It would be important to identify households where families have been able to organize themselves to ensure that the mother/child pair were more often together than apart. Showcasing how different families have organized themselves to ensure that mothers are close to their children so that they can breastfeed exclusively up to six months would be key, building on existing positive practices.
4.2.3 Promoting Regular Intake of IFA and Iron-Rich Foods During Pregnancy and Postpartum—Addressing the Fear of Having Too Big of a Baby
It is critical to consider how best to create an understanding of the need to take IFA regularly during pregnancy and the postpartum period. Women know that these tablets “make them strong” but many don’t take them regularly, for a variety of reasons. One is that the ANM does not prescribe nor counsel the pregnant women regarding the IFA. The nutrition videos should focus on creating demand from the client, to ensure that IFAs are prescribed. Women also reported, however, not taking IFA because of the “bad taste,” the common side effects, or because of the fear that their child will be too big. Others reported taking them because they know and their child will be healthier. Creating messages to promote IFA needs to be done in partnership with ANM and ASHAs to ensure not only that women are empowered to ask for the tablets, but also that IFA is prescribed according to protocol. In addition, it was clear from the interviews with mothers and mothers-in-law, that although there is a perception that IFA consumption during pregnancy is associated with “too big of a baby and difficult delivery,” many respondents were actually not sure and were discussing among themselves and asking the researchers whether that was true or not. There appears to be an openness in the community and an interest in learning more about IFA, which the community video project can build on. Since this openness is most probably due to the messages being given by the ASHAs and ANMs, it would be key to engage them in actually addressing women’s fear of having too large of a baby in the videos promoting regular IFA consumption during pregnancy.
In addition to promoting IFA consumption, the program can link nutrition-focused videos with the agricultural videos that promote kitchen gardens; for example, the promotion of enriched complementary foods, explaining the importance of eating spinach and other green leafy vegetables to promote the dietary intake of locally available high-iron-content foods. If the nutrition-focused videos are linked with videos promoting the adoption of kitchen gardens, this could help to promote the adoption of new agricultural practices as well.
4.2.4 Promoting the Health of Breastfeeding Mothers
During the research, many mothers-in-law and breastfeeding mothers reported food intake restrictions during the breastfeeding period to ensure that the baby does not have stomachaches. However, as mentioned before, times are changing, and messages about healthy eating during breastfeeding are being promoted by ASHAs and ANMs. Mothers themselves are expressing concerns about being hungry. The findings indicate that there is more openness now for changing the behaviors around food intake restriction, if there is more discussion/explanation of the mother’s need for food, for her own body and the body of the child. An explanation can be given that once the child has received enough milk to meet his or her needs, the child stops suckling, but that the mother needs increased energy to keep making more milk.
4.2.5 Complementary Feeding
Pregnant women, breastfeeding mothers, husbands, and mothers-in-law reported openly not really knowing when to introduce complementary foods and how to introduce such foods. All respondents asked for advice and expressed their need to learn more—a critical step leading to behavior change. It is clear that there is limited understanding of food consistency (everyone reported giving watery dhal) so messages about consistency and demonstrating consistency through the videos should be a priority. Questions about frequency also appeared in the research, with indications that most children eat when adults eat, and when hungry in between meals, are given rice cakes containing little or no nutritional value. Cooking specific foods for children does not appear to be a current practice. Identifying households who have introduced other nutritious foods to enrich the “watery dhal” would be a key priority. Researchers saw a few households that are adding mashed chickpeas to the dhal and this would be a positive example of a practice that could be promoted at scale.
4.2.6 Enriching Complementary Foods with Locally Grown Foods
As the SPRING/Digital Green collaboration is focused on trying to understand how feasible it is to introduce nutrition messages within an existing agricultural platform, this might be one of the best opportunities to build synergy. Nutrition videos related to enriching the foods given to babies could complement the agricultural videos about promoting kitchen gardening and small-animal rearing. The nutrition videos could share how best to improve the quality of the rice/dhal, or other complementary foods, reinforcing the messages from the agricultural perspective. The nutrition information might help foster rapid adoption of new agricultural practices, especially if farmers understand how these new crops can help the health of their families. Creating and distributing the videos will require close planning with VARRAT, the local implementing partner, in defining a schedule for video production/dissemination that harmonizes the nutritional and agricultural messages.
4.2.7 Strengthening the Role of Husbands as Supportive Partners
Many women shared that in times of need, they would turn to their husbands. When interviewed, husbands shared that they felt a sense of responsibility for their wives and children. These findings seem to confirm that husbands play an active role in the family. Husbands did not, however, seem to know much about optimal MIYCN practices, including the importance of IFA during pregnancy or exclusive breastfeeding up to six months. Specifically, findings from the four in-depth interviews with fathers showed that they were specifically influenced by marketing practices promoting infant formula. Informing fathers—either through the agricultural videos dissemination sessions or separate disseminations—about appropriate complementary feeding and exclusive breastfeeding might be a strategy to strengthen the supportive roles of fathers.
4.2.8 Enhancing the Role of Mothers-in-Law in Childcare Practices
As stated before, mothers-in-law are aware that times are changing. As shared during the focus group discussion with mothers-in-law, they also want to play a more supportive role in helping care for their daugthers-in-law and the grandchildren. They shared that they were relieved that times were changing compared to when they were young mothers, when it was very difficult for them in terms of eating enough foods and having time to rest. At the end of the FGD, mothers-in-law shared that they did not know enough about complementary foods and also about how to “be a good grandmother.” Of the four grand-mothers interviewed, one explained how her daughter-in-law eats with her and how she ensures she has enough foods. She also explained that for her, as a grandmother, she wants to make sure her grandchildren are safe and well taken care of. The other three grandmothers explained that videos showing how to take care of very young children would be helpful, as at times they are not sure what to do. Videos that promote active feeding, encouraging the child to eat when not hungry, and spending time with the child during meals would be helpful.
4.2.9 Exclusive Breastfeeding During the First Six Months of Life
Because it will be difficult to build an understanding that the child does not need any extra food or water other than breast milk until the sixth month, identifying mothers in the communities who actually exclusively breastfed their children up to the six month will be key. During the research, such mothers were identified in the group of women who lived within the households with some access to education. Engaging these positive-deviant mothers and their families (mothers-in-law and supportive husbands) as “stars” in the videos should be one of the strategies used. One has to realize, however, that exclusive breastfeeding up to six months will be difficult to promote for several reasons, including the limited belief that breast milk is enough during hot season; and the fact that many women have to go back to work in fields that are far away from the home after 21 days. Discussions about shifting the labor responsibilities of new mothers from labor in the field to labor within the home might help to ensure that children can be breastfed exclusively.
4.2.10 Handwashing with Soap
Although a lot has been written about the importance of handwashing to protect infants and young children from deadly diarrheal diseases, it is clear from the research that there is a wide gap between the knowledge of the importance of handwashing and its actual practice. Currently, UNICEF India is focusing heavily on hygiene, and has developed a video promoting handwashing with soap that can be downloaded on mobile phones, which is a potential area of synergy or collaboration. When visiting homes, our observers found that soap was seldom available and noted buckets of water with small pitchers, but not strategically located near food preparation and eating areas. Open defecation and limited handwashing continue to promote diarrheal diseases in the communities surveyed, as shared by the Panchayat leaders. Tackling the larger problems associated with compound hygiene and the use of latrines is beyond the scope of this short collaboration, but the promotion of handwashing with soap, with emphasis on doing so before preparing foods and before eating or feeding infants and young children, is believed to be feasible and appropriate within the objectives of this collaboration.
5. Conclusions and Recommendations
The following list summarizes the major conclusions and recommendations that emerged from careful analysis of the key MIYCN-related behaviors and the formative research findings.
- An overall recommendation is to develop videos that address nutrition-related issues focused on the 1,000-day framework, since the formative research shows that serious nutrition issues, as well as sociocultural and economic barriers, exist at each stage—from pregnancy through the first two years of life.
- It is critical to address maternal nutrition during pregnancy, promoting one extra meal, promoting rest, and strengthening adherence to recommended IFA supplementation by addressing some of the misconceptions identified during the research such as food taboos. During video production, it will be important to engage with the ASHAs, AWWs, and CSPs to identify how best to address the deeply embedded food taboos that may be harmful. (Not every taboo is harmful, and it is therefore necessary to select only those taboos that need to be addressed.) It is important as well to acknowledge but not confront taboos that are not harmful, in order to engage in a “compromise” with the community.
- Although early initiation (within one hour) is reported as being a universal practice, exclusive breastfeeding up to six months is not. As identified in the research, within the first few weeks of life, rice cakes, honey water, water, and gripe water are usually introduced. The practice varies from introducing tastes of food within the first few weeks to introducing multiple foods by the third or fourth month. Videos explaining that breast milk provides sufficient liquid to the baby, even during the hot months; that women make more milk when the child breastfeeds; and that when a child is ill, he or she needs to be breastfed more often, are all priority topics. Identifying women in the community who practice these behaviors consistently may be a challenge, as most women go back to the field and end up leaving their children with other caregivers or mothers-in-law, who often introduce some type of snack or alternative milk until either the mother returns or the child is brought to her in the field.
- Most respondents shared that videos teaching mothers about complementary foods are essential. Respondents across the groups shared that mothers only feed watery rice, watery dahl, or sometimes just water with salt, and that there is limited understanding about the appropriate consistency and frequency of feeds. Thus, several videos showing how to improve the quality of complementary foods are crucial. One of the strategies to promote greater integration between the agriculture and nutrition video disseminations is to review with the VARRAT team the agricultural videos schedule, so that those videos that specifically promote kitchen gardens, vegetable growing/horticulture, and/or small animal husbandry can be followed the next week with a nutrition promotion video. For example, if in one week, an agriculture video shows how to grow pumpkin, the next week, the video might be about how to use cooked pumpkin to enrich complementary foods, such as the “watery rice” currently given to children.
- Handwashing with soap has been identified as a key practice to promote, with special emphasis on handwashing before preparing foods and before eating or feeding infants and young children. All respondents reported knowing the importance of hand washing, but, nevertheless the practice of handwashing is not common. One issue is that although there are water pumps in most villages, homes do not have easy access to piped water. Women generally have to fetch water in pots, which they need for cooking and washing. Introducing a new technology such as tippy taps can be tested. The construction of simple handwashing stations, and perhaps tippy taps, should be promoted in areas of the home that are convenient for handwashing.
- Mothers-in-law should be specifically targeted when developing nutrition promotion videos, since they are powerful decision makers and gatekeepers in the households. They need to be engaged and convinced about the importance of promoting optimal MIYCN. If mothers-in-law are not convinced that behavioral change is needed, it will be difficult for the pregnant women and breastfeeding mothers to actually change their own practices within the family. Actively engaging the mothers-in-law is key.
- Husbands and fathers also need to be engaged in video viewing and discussions. Throughout the research, husbands were described as supportive of their wives, but not able to make decisions contrary to their own mothers’ views. Specifically tailored videos, allowing viewing with other men, might be an effective strategy to enhance discussions and promote changes within the household.
- Engaging the community health agents—ASHAs and AWWs—in the reviewing of the content of the videos, and perhaps as “stars” in the videos, is highly recommended given their specific role in the community. A community-based review committee could be considered where representative ASHAs, AWWs and Panchayat leaders have the opportunity to review video content or draft videos in order to ensure that they align with the key messages promoted by the nutrition community in Odisha. Also, by including the Panchayat leaders, this will not only help ensure that the videos align with some of the Panchayat health priorities, but they might also increase Panchayats’ commitment to address health issues at the community level.
Footnotes
1 The scheduled castes, scheduled tribes, and other backward classes are official designations given to various groups of historically disadvantaged people in India and recognized in the constitution.
2 Mamata Diwas: “Mothers’ Days” are days where the AWWs share information on child health and maternal health, promoting family planning, child immunization, hygiene and sanitation. Nutrition Days take place once a month. During Nutrition Day, children under five years are weighed and measured, and mothers receive nutrition advice.
References
Coalition for Sustainable Nutrition Security in India. 2008. Essential Interventions for Reducing Malnutrition in Infants and Young Children in India: A Leadership Agenda for Action. New Dehli: Coalition for Sustainable Nutrition Security in India.
Government of Odisha. 2012. District Profile. Bhubaneshwar, Odisha: Government of Odisha. http://ordistricts.nic.in/district_profile/aboutus.php (accessed September 2012).
International Institute for Population Sciences (IIPS) and Macro International. 2007. National Family and Health Survey (NFHS-3), 2005–06: India: Volume I. Mumbai: IIPS.
International Institute for Population Sciences (IIPS) and Macro International. 2008. National Family and Health Survey (NFHS-3), 2005–06: India: Orissa. Mumbai: IIPS.
Maps of India 2014. Odisha District Map. www.mapsofindia.com. Accessed June, 2016. http://www.mapsofindia.com/maps/orissa/orissa.htm
Mehta, S. K. 2011. Including Scheduled Tribes in Orissa’s Development: Barriers and Opportunities. Children of India: Rights and Opportunities, Working Paper No. 9. New Dehli: IHD/ UNICEF.
Ministry of Health and Family Welfare. 2013. A Strategic Approach to Reproductive, Maternal, Newborn, Child, and Adolescent Health (RMNCH+A) in India. New Delhi: Government of India.
Ministry of Home Affairs. 2011: Annual Health Survey 2010–11: Fact Sheet, Odisha. New Dehli: Government of India. Available at http://www.censusindia.gov.in/vital_statistics/AHSBulletins/AHS_Baseline_Factsheets/Odisha1.pdf (accessed September 2012).
MS Swaminathan Research Foundation (MSSRF)/World Food Programme (WFP). 2008. Report on the State of Food Insecurity in Rural India. Chennai: MSSRF/WFP.
Naandi Foundation. 2011. HUNGaMA Survey Report 2011. Hyderabad: HUNGaMA/Naandi Foundation.
Office of the Registrar General & Census Commissioner, Ministry of Home Affairs. 2011. Annual Health Survey: Odisha 2010–11. New Dehli: Government of India.
Office of Registrar General, Vital Statistics Division. 2013. Special Bulletin on Maternal Mortality in India 2010-12: Sample Registration System. New Delhi: Government of India.
Panigrahi, A., and P. B. Sahoo. 2011. “Nutritional Anemia and Its Epidemiological Correlates among Women of Reproductive Age in an Urban Slum of Bhubaneswar, Orissa.” Indian J Public Health 55(4):317–20.
UNICEF. 2012. Odisha State Profile. Geneva: UNICEF. Available at http://www.unicef.org/india/state_profiles_4346.htm (accessed September 2012).
UNICEF. 2013: “Nutrition.” Geneva: UNICEF. Available at http://unicef.in/Story/1124/Nutrition (accessed January 2013).
Viteri, F. E. 1994. “The Consequences of Iron Deficiency and Anemia in Pregnancy.” Adv Exp Med Biol 352:127–39.
World Heatlh Organization (WHO). No date. Anaemia Data by Country. Geneva: WHO. Available at http://www.who.int/vmnis/database/anaemia/countries/en/ (accessed January 2013).


