Current analysis of maternal and child nutrition programs is often confined to looking at a few direct outcomes over a set period of time, such as change in nutritional status or pregnancy outcomes–occasionally analysis extends to changes in mortality in the near term period. However, given our growing understanding of the importance of fetal and early life growth and nutritional status on later health outcomes, more evidence is available that suggests interventions that impact health and nutritional status in the 1,000 days period can have significant benefits beyond the immediate term, and to limit estimation of benefits to childhood outcomes significantly risks underestimating the cost effectiveness of such interventions.
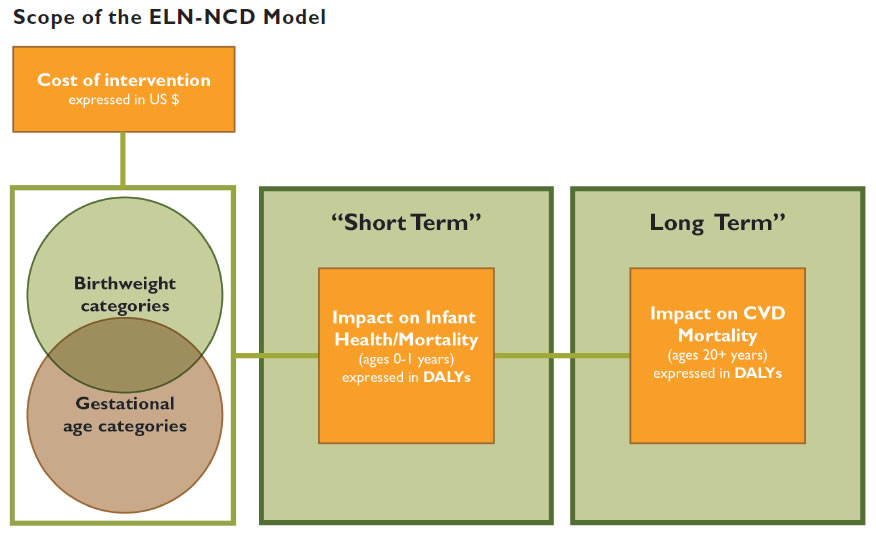
USAID asked SPRING to develop a simulation model that aims to produce a more inclusive understanding of the relative value of nutrition interventions by extending the time frame for estimating treatment benefits, most specifically in terms of quantifying the "value added" by their impact on early life genetic programming and any resulting later life course nutrition-related NCD risk.
This area is of particular interest due to the growing evidence of the ballooning burden of NCDs on "transitioning" low-to-middle income countries and the implications for health care expenditures.
SPRING has completed the first phase of the model, which looks at selected maternal nutrition and health interventions that affect birth weight and gestational age in Bangladesh (see the phase I report below). Using evidence review, expert consultation, and multiple country- and region-specific datasets, SPRING gathered the best available evidence on the costs of interventions, effects of interventions on birth outcomes, and how those birth outcomes then affect the relative risk of acquiring a nutrition-related NCD in adulthood in this country context.
This information was used to develop a multi-level simulation model to estimate lifetime health burden based on birth outcomes across a series of categories of birth weight and gestational age. When combined, the model’s results produce cost-effectiveness ratios (CERs) which allow comparison of each intervention’s impacts and present a more complete measure of “value for the money,” or benefits per dollar, than traditional CERs that only account for short term effects. After the first phase is complete, USAID and SPRING will explore where the model can be expanded to include other interventions, other countries, or potentially other nutritional pathways.
Results from the model will be posted on this website as they are completed, so please keep checking back for further information. Also check out SPRING’s other work on nutrition-related NCDs, including country and region profiles that explore where future risks may lie in low-to-middle income countries.
