A Landscape Analysis of Anemia and Anemia Programming in Uganda
Background
Anemia, or low levels of hemoglobin, is one of the most common public health problems in the world today. It affects 25 percent of the world’s population, more than 1.6 billion people (Benoist et al. 2008). About half of all anemia is due to iron deficiency, a condition caused by inadequate intake or low absorption of iron. Iron deficiency anemia (IDA) alone contributes to more than 100,000 maternal deaths and almost 600,000 perinatal deaths each year (Stoltzfus et al. 2004). Other causes of anemia include micronutrient deficiencies, intestinal helminthes, malaria, HIV infection, and hemoglobinopathies. Iron deficiency anemia and iron deficiency increase the risk of prematurity, preterm delivery, low birthweight, and maternal and child mortality; they reduce the cognitive and physical development of children, causes fatigue, and reduce the physical stamina and productivity of people of all ages. The prevalence and burden of anemia disproportionately affect young children and women of childbearing age (particularly pregnant women) in Africa and South Asia (Stevens et al. 2013).
In Uganda, anemia has been a major public health problem for many years. The earliest nationally representative anemia data are from the 2001 Uganda Demographic and Health Survey (UDHS). They indicated that 71 percent of children under five and 37 percent of women of reproductive age (WRA) were anemic. Five years later, these rates increased to 73 percent and 42 percent, respectively (Uganda Bureau of Statistics and ICF International, Inc. 2007). According to the World Health Organization (WHO), countries in which the national anemia prevalence rate is 40 percent or more have a “severe” public health problem. Since 2006, however, Uganda has made considerable progress in this area. The 2011 UDHS reported prevalence rates of 49 percent and 23 percent among children and WRA, respectively. This reflected reductions of 32 percent and 45 percent, respectively, and surpassed the Government of Uganda’s (GoU) targets for 2016 (GoU 2011).
Rationale for the Study and Study Objectives
The purpose of this study was to better understand the factors contributing to the reduction in anemia prevalence and to inform anemia, nutrition, and health policies going forward. This included assessing the changes in the nature, coverage, and utilization of programs, as well as assessing changes in personal practices and behavioral patterns of Ugandan children (6–59 months old) and WRA (15-49 years old) over the past decade. Another objective of the study was to deliberate and develop consensus among stakeholders about which programs most likely contributed to reducing anemia. It was also hoped that this analysis would promote the development of a long-term participatory process of cross-program and multisectoral coordination that would encourage more integrated policy and program approaches that will improve the coverage, effectiveness, and efficiency of anemia-reductions efforts.
The specific objectives of the study were to—
- assess the plausibility that key anemia control and prevention programs contributed to the decline in anemia among children 6–59m and women of childbearing age by looking at changes in program coverage between 2001 and 2010
- foster an environment that encourages discussions about implementation challenges to anemia prevention and control efforts in Uganda.
Research Design and Methods
This study analyzed data from three UDHS surveys conducted in 2000-01, 2006, and 2011. In each survey, hemoglobin was collected and anemia prevalence was established. Hemoglobin levels were adjusted for altitude and were calculated separately for children 6–59 months and of women 15-49 years of age.
This study assessed trends in anemia and explored the plausibility of different programs having played a role in affecting the prevalence of anemia in two distinct populations: women of reproductive age (WRA) and children. Given that the types of anemia-related programs targeted to each of these populations differ, the discussion is structured into independent analyses of each of these populations.
Findings: Maternal Anemia
- WHO considers anemia to be a mild, moderate, or severe public health problem if prevalence among women is 5–19 percent, 20–39 percent, and greater or equal to 40 percent, respectively. After initially increasing from 36 percent in 2001 to 41 percent in 2006, the prevalence of anemia among WRA fell to 23 percent, making anemia a moderate public health problem in Uganda in 2011. More than two-thirds of the 18-point reduction in the prevalence of anemia between 2006 and 2011 was due to reduction in mild anemia.
- In 2011, anemia prevalence was lowest among women from the Western region, those with higher education, women who lived in urban areas, and women from the middle wealth quintile. The highest decline over the decade was seen among women living in the Western region. While the prevalence of anemia in Central and Eastern regions fell by one-third, in the Northern region, the proportion of anemia fell by 44 percent (leaving it with the second lowest in 2011), and Western rates fell by 63 percent. Another notable change from 2001 to 2011 was that differences in rural and urban women’s anemia rates dramatically narrowed. While urban areas made significant progress—reducing anemia by about five percentage points during this period—the progress in rural areas was three-fold greater, as rural rates fell by 15 percentage points.
- Anemia in pregnancy remains a serious public health problem in Uganda. Antenatal care (ANC) is a widely used strategy to improve the health of pregnant women and serves as a platform for many maternal anemia interventions such as provision of deworming medicine, iron–folic acid (IFA) supplements, intermittent preventive treatment of malaria in pregnancy (IPTp) and distribution of insecticide-treated nets (ITN).1 The Ministry of Health (MOH)’s ANC program, therefore, provides a particularly powerful mechanism for reaching the vast majority of pregnant Ugandan women.
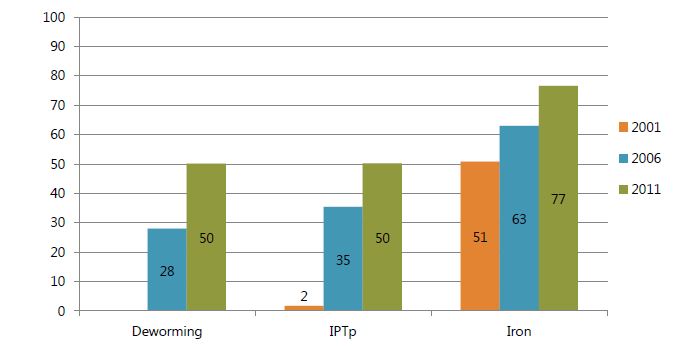
- In 2001, ANC coverage was 94 percent and had reached 96 percent by 2011. However the first ANC visit continued to occur late in pregnancy, at five months. The percentage of women receiving any iron supplementation during pregnancy increased from 51 percent in 2001 to 77 percent in 2011. Similarly, the percent of women receiving any dose of IPTp rose from 2 to 50 percent over the same time period. Although the 2001 survey did not ask about deworming drugs, between 2006 and 2011 the proportion of women who received at least one dose during pregnancy nearly doubled. Despite the increase in ANC coverage, less than 10 percent of women were receiving the two or more doses of IPT, and less than half were receiving deworming medicine, indicating that policymakers may not understand the benefits of the anemia interventions in the ANC platform in Uganda. In addition, although the proportion of women receiving any iron supplementation improved steadily over the past decade, progress in the number of IFA tablets distributed has been slow.
- Apart from promotion of sleeping under an ITN and promoting iron-rich food consumption, Uganda does not implement targeted anemia prevention and control strategies for WRA outside ANC. IFA for adolescent girls is included in Health Sector Strategic Plan III, which has not yet been implemented in Uganda.
Figure 1. Among Women with a Birth in the Past Five Years, Percentage Reporting Receiving Various Anemia-Related Interventions during Pregnancy, 2001–2011
- Bed net ownership in Uganda increased from 42 percent in 2001 to 80 percent in 2011, and the proportion of women sleeping under bed nets the night before the survey more than doubled, from 26 to 55 percent. The increase in bed net ownership between 2001 and 2011 was accompanied by a modest increase in the rate of bed net use by owners, from 62 percent to 69 percent. Table 1 shows regional differences in bed net data. In 2001, the level of ownership of bed nets in the Western region was one-third the rate of the rest of the country. By 2006, the Western region had narrowed the gap, but its ownership rate was still only slightly more than half the rate in the rest of the country. Over the next five years, ownership rates surged in all regions of the country; those in Western outpaced all other regions and came to have a rate that surpassed that of Eastern and was equal to the national average of 80 percent.
Table 1. Proportion of Non-Pregnant Women Owning a Bed Net, and among Those Who Own, the Percentage Who Slept Under One the Previous Night, by Region, 2001–2011
| 2001 | 2006 | 2011 | ||||
|---|---|---|---|---|---|---|
| Ownership | Use | Ownership | Use | Ownership | Use | |
| Central | 16.9 | 44.8 | 48.3 | 58.8 | 84.1 | 67.7 |
| Eastern | 17.5 | 73.8 | 38.9 | 76.4 | 73.9 | 73.4 |
| Northern | 17.1 | 72.6 | 45.8 | 56.4 | 83.6 | 73.0 |
| Western | 5.7 | 43.0 | 25.6 | 62.3 | 79.8 | 62.1 |
| Total | 14.3 | 61.0 | 39.1 | 63.1 | 80.1 | 68.6 |
Findings: Child Anemia
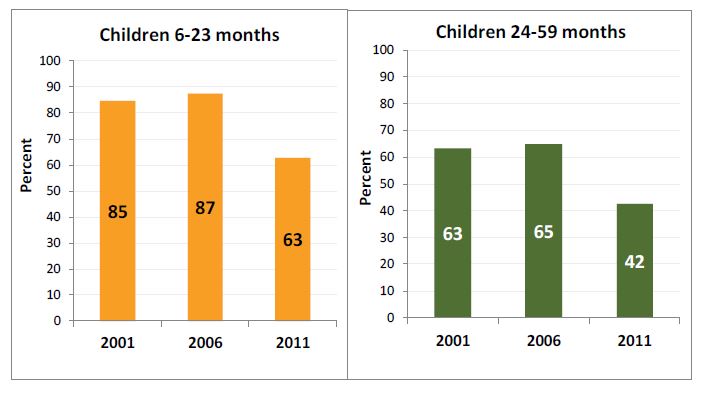
- Anemia among children between 6–59 months increased slightly from 2001 to 2006, but declined significantly by 2011 (Figure 2). Among children 6–23 months, the prevalence of anemia did not change, but declined to 63 percent in 2011. Prevalence of anemia among children 24–59 months is lower, but shows a similar declining trend.
Figure 2. Anemia Prevalence among Children 6–23 Months (Left) and Among Children 24–59 Months (Right)
- In 2011, in both children’s age groups, the prevalence of anemia varied significantly by highest educational level of mother, household wealth quintile, and region. The prevalence of anemia among children 6–23 months old whose mothers had no education showed a decrease from 86 percent in 2001 to 60 percent in 2011. Similarly, the prevalence of anemia among children 24–59 months old whose mothers had no education showed a decrease from 68 percent to 45 percent. The decline of anemia in both age groups was highest among children who belonged to the highest two wealth quintiles. Although Western children experienced the largest percentage point and percentage reductions in anemia prevalence from 2006 to 2011, they were already the lowest in 2001.
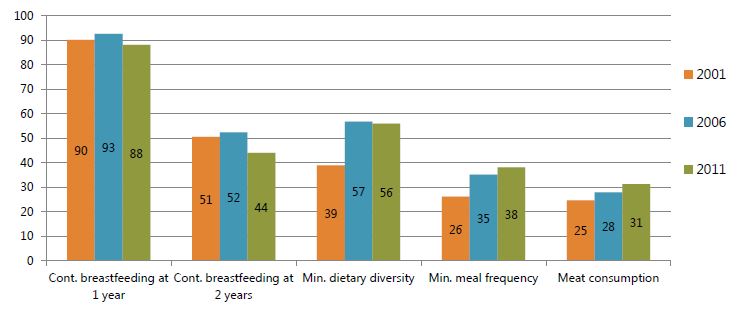
- Figure 3 summarizes trends in five selected indicators of feeding practices and dietary patterns that effect IDA in children 6–23 months: continued breastfeeding at one year; continued breastfeeding at two years; minimum dietary diversity; minimum meal frequency in the past 24 hours; and consumption of meat in the past 24 hours (as defined by WHO).2 The figure above suggests that while breastfeeding rates have deteriorated over time, there have been marginal improvements in the other three infant and young child feeding practices over the last decade.
Figure 3. Feeding Practices and Dietary Patterns of Children 6–23 Months
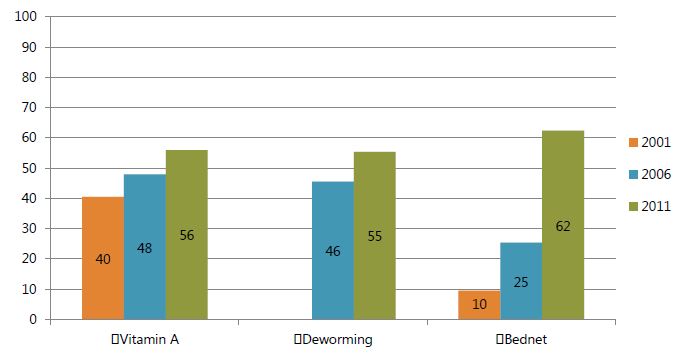
- Figures 4 and 5 show trends in the participation of children in three anemia-related programs. The coverage of all three programs has grown each year, with the exception of vitamin A coverage among the younger children from 2006 to 2011. By far, the most dynamic program has been bed nets. Bed nets had the highest growth rates of any program in any year, and in the most recent survey in 2011, was the program with the highest coverage rate. The next-highest rate was that of vitamin A supplementation coverage. While the rate among the older children has increased, its pace lagged behind that of the younger age groups in 2006 and 2011. Although vitamin A coverage rates fell among the 6–23 month olds in 2011, it continued increasing among 24–59 month olds. Among the older children, the rates of coverage of deworming and vitamin A have varied by only one or two percentage points and have moved in tandem. The deworming rates have been relatively lower among the younger group, reflecting the fact that the program is limited to children 12 months of age and older.
Figure 4. Among Children 6–23 Months, Prevalence of Select Anemia-Related Behaviors, 2001-2011
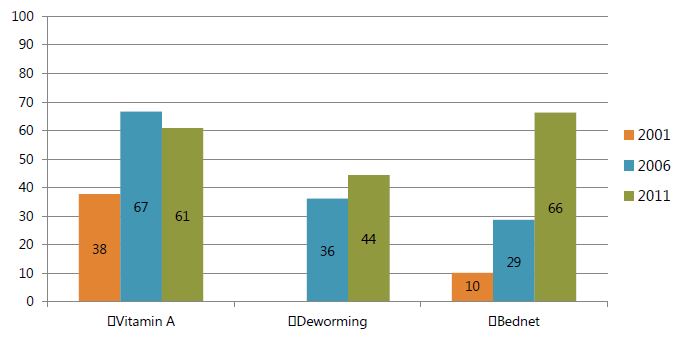
Figure 5. Among Children 24–59 Months, Prevalence of Select Anemia-Related Behaviors, 2001–2011
Discussion
Uganda has shown a remarkable reduction in anemia prevalence over the last five years. The reductions in anemia among children 6–59 months and among WRA reflect broad-based gains by all strata of the population since 2006 that more than offset the 2001-2006 increases in prevalence rates.
The findings from this study show that while the gains since 2006 have been enjoyed widely, the rates of decline in anemia prevalence have varied, with some groups and strata experiencing relatively greater gains. Most of women’s gains have been in mild anemia, whereas among children—especially among the youngest children, 6–23m—there have been larger percentage point reductions and larger percentage declines in moderate and severe anemia. Based on the findings, several behaviors and programs may have contributed to reduction in prevalence of anemia among women and children over the last 10 years.
- Substantial increases in behaviors related to anemia reduction were seen in the large-scale ownership and use of insecticide bed net use among both WRA and children under five.3 The changes in bed net use increased by 45 percentage points among women and 52 percentage points among children 6–59 months between 2001 and 2011.
- Among 6–59 months, there was a remarkable growth in the number of anemia-related programs and behaviors in which Ugandan children engage. In 2001, 43 percent of all 6–23 month olds and 48 percent of 24–59 month olds did not receive any anemia-relevant services. These percentages fell dramatically over the following decade, reaching roughly one-fifth that level in 2011, reflecting a major transformation in Ugandans’ health-seeking behavior patterns. In 2006, the percentage of older children who did not participate in any program was 25 percent, nine percentage points higher than rate of younger children who did not participate in any programs, which was at 16 percent. At the same time, the number of children participating in all three programs went from nine to approximately 25 percentage points in 2011. Considering the three programs that children in both age groups have in common—deworming, vitamin A supplementation, and bed nets—among 6–23m olds, the average (mean) number of programs has gone from 1.31 in 2006 to 1.63, an increase of 24 percent, and among 24–59m olds, it has increased even more; from 1.28 to 1.71, an increase of 34 percent among children 6–23 months.
- The proportion of women receiving the three anemia-related ANC services also changed impressively in the last decade. In 2006, 12.7 percent of women reported that they had received IFA and IPTp services during their last pregnancy. In 2011, the percentage of women reporting they had received any two services increased from 26 to 3 percent. The percentage of women who reported receiving all three services more than doubled, from 11 percent in 2006 to 27 percent in 2011. The significant variation in the combinations of these services and the changing patterns with which they have been provided suggest that although the performance of ANC has improved steadily in the last decade, there remains substantial room for improvement.
Study results indicate that several strategies for anemia prevention and control are in place in Uganda. These include supplementation of women and children with iron and vitamin A, deworming, food fortification (particularly vitamin A-fortified oil), and strong malaria prevention and control programs. The proportion of women and children participating in anemia-related interventions has also increased in the last decade. However, a number of challenges to sustaining and improving these programs remain. The low coverage and participation of women and children in integrated maternal and child health programs may indicate a number of challenges with such programs, including issues related to quality of services, human and financial resources, provider capacity, awareness of anemia and related services, and other factors that may hamper the effective delivery of these services.
Despite having the focused ANC package and Child Days Plus (CDP) programs in place, the Ugandan health care system has not been able to fully commit to ensuring that all components of the package are implemented for a majority of the target populations. Poor financial resource allocation, inadequate human resources, poor management and quality of care are possible factors that confound the implementation of various integrated package components (Health Sector Strategic Plan II).
Download the PDF above to read the full report.
Footnotes
1 Use of insecticide-treated nets (ITNs) is also recommended and the National Malaria Control Program’s Strategic Plan calls for ITNs to be distributed during antenatal care clinic visits, but the DHS only asks about bed net use during the night prior to the survey, not during pregnancy.
2 Three IYCF practices (per breastfeeding) status refers to infant and young child feeding practices among children 6–23 months old living with their mothers, as established by WHO. The binary indicator takes into account food diversity (number of food groups), frequency of feeding; and consumption of breast milk or other milks and milk products and is restricted to the last-born child.
3 It is important to highlight that bed net ownership and use questions were based on questions that asked about use the night before the interview, while other questions were based on use of services in the last five years before the survey. So there may be a slight recall bias with regard to some of the other service-use responses.
