Findings from SPRING's Micronutrient Powder (MNP) Distribution Pilot Program in Uganda

Introduction
As program managers and researchers consider ways to improve the evidence base for nutrition decision-making in low and middle-income countries (Pitt et al. 2016), it is important to carefully consider the costs and cost-efficiency of alternate nutrition programs and health promotion initiatives (Belli 2001). Economic evaluations of health care interventions involving costing studies and analysis of intervention outputs (performance) and outcomes (effects) help provide insights into the complete costs of health and nutrition interventions. As Horton, et al. (2009) illustrates, the financial resources necessary for addressing nutritional deficiencies in the 36 most affected regions of the world are staggering, at $10.3 billion a year. If policymakers know what interventions actually cost, as well as the expected population coverage and impact of interventions, these studies can help build an economic case for policymakers to prioritize nutrition interventions that have the highest population coverage and the potential greatest results with limited resources (Baker et al. 2015). There are various types of economic evaluations of health and nutrition programs that can be conducted, and they differ based on the inputs and outcomes used, or the metrics of comparison (Box 1). In this brief, we present results from a cost-efficiency study of a pilot program of micronutrient powder (MNP) distribution in Namutumba district in Uganda. We consider this a cost-efficiency study because we did not measure hemoglobin, which is the biological outcomes that will be influenced by consumption of MNP. This brief discusses costing studies for nutrition interventions generally, and highlights how a cost-efficiency study can influence policy decisions.
Box 1: Types of Economic Evaluations
- Cost Analysis: This is a comparison of costs between two programs, and this does not include a measurement of biological outcome or any indicator that measures the impact. In our brief, we refer to this study as a cost-efficiency analysis.
- Cost-benefit analysis: In this type of economic evaluation, the inputs and outcomes are expressed in the same units, which is usually money.
- Cost-effectiveness analysis: In this type of economic evaluation, the inputs and outcomes from two programs or interventions are compared using a metric of cost per unit of health or nutrition outcome.
- Cost minimization analysis: In this type of economic evaluation, the impact of two programs is the same, and the comparisons are only made within the cost inputs.
- Cost-utility analysis: This study design is used to compare two programs that have different outcomes that are expressed as 'utilities', e.g. disability-adjusted life years.
Source: National Information Center on Health Services Research and Health Care Technology (NICHSR). Health Economics Information Resources: A Self-Study Course available here.
How to Measure “Cost” in a Cost-Efficiency Study
Cost-Efficiency is the measure of compliance of a program according to criteria of acceptable performance or effect per unit of cost incurred. Cost-efficiency indicators for a given intervention can include: cost per dose distributed, cost per beneficiary reached, and cost per beneficiary effectively adhering to an established protocol. There are a number of costs to consider when conducting a costing and cost-efficiency study (Box 2). We present the costs in three different categories, budgetary costs, opportunity costs, and total costs.
Box 2: Key Costs in Cost-Efficiency Analysis
Budgetary costs: cost of all program inputs in the program budget, including all capital investments, start-up costs, and outlays for recurring and ongoing implementation activities.
- Capital investments: purchases of equipment, vehicles, training, and office materials, for example.
- Start-up costs: program activities carried out in order to initiate an intervention. These expenses are incurred before a program begins.
- Recurring costs: repeated costs incurred regularly. These might include fixed costs such as rented office space and the regular purchase of micronutrient doses.
- Ongoing activity costs: the cost to a program for operations such as monitoring, support, supervision, and outreach.
- Opportunity costs: non-budgeted costs faced by caregivers and others who volunteer their time, calculated in terms of foregone earnings from alternative economic activities.
- “Last Mile” costs: costs incurred during the final leg of service/product distribution to the beneficiary. Most of these costs are comprised of the opportunity costs of health workers, volunteers, and caregivers.
Total costs: the sum of budgetary and opportunity costs for the entire program.
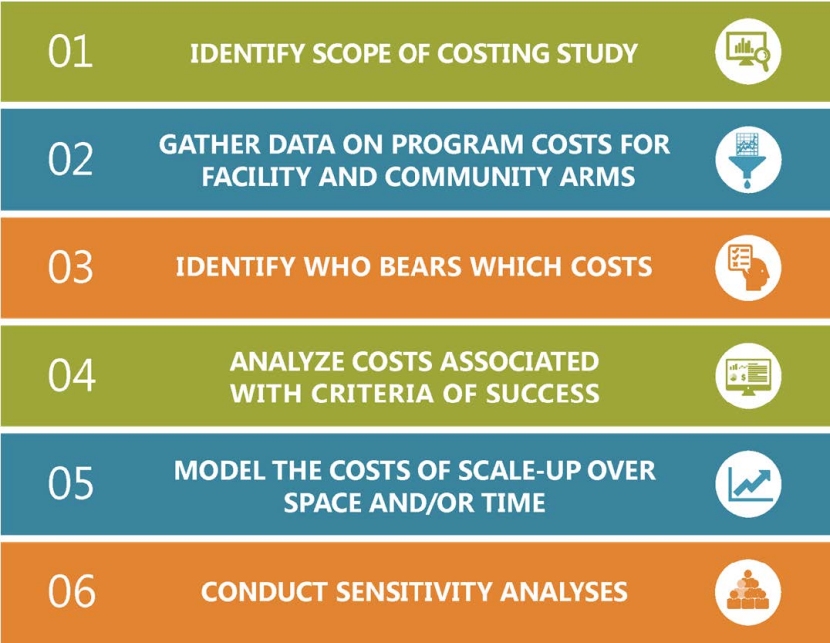
The following is a set of guidelines developed by Hendriks, et al. (2014) for conducting an economic evaluation of costs and outputs (Box 3).
Box 3: Guidelines for cost-efficiency studies
- Set the scope of the study by defining the problem facing decision makers, including the objectives and measures of success for the program (i.e. criteria to qualify performance).
- Define the unit of analysis based on the scope that has been set.
- Determine which costing items, including activities, personnel, logistics, or capital investments, will be involved in a given intervention and hence require data collection.
- Quantify cost items through time allocations for personnel or beneficiary time, distribution records, and transportation logs.
- Determine the value of each cost item, whether through a “top-down” approach using financial statements, or through a “bottom-up” approach using the number of beneficiaries multiplied by an estimated unit cost of service/product provision.
- To account for uncertainty or variability in program costs and implementation, consider a range of potential optimistic and pessimistic scenarios (compared to the base model) and conduct sensitivity analyses on all cost-effectiveness measures.
When comparing estimated costs against estimated outputs to arrive at cost-efficiency measures, it is important to remember that different measures of the output will generate different cost-efficiency estimates. This implies that the selection of the indicator to be considered as an output of the program will be the critical criterion in interpreting the ranking of the alternative programs being compared. The next section demonstrates how these guidelines were applied in the context of a micronutrient powder distribution costing study conducted in rural Uganda.

A Micronutrient Powders Costing Study in Uganda: Rationale and Methods
Iron-deficiency has consequences for long-term cognitive and behavioral development (Krebs et al. 2017; World Health Organization 2001). One consequence of iron-deficiency is anemia, and although anemia might be caused by many other factors, it has been commonly used to predict the magnitude of iron-deficiency. Anemia affects nearly 9.6 million children ages 6-59 months worldwide (World Health Organization 2015). In Uganda, it has been estimated that anemia affects 53 percent of children ages 6-59 months and 32 percent of women ages 15-49 years (Uganda Bureau of Statistics and ICF 2017). The Government of Uganda has a commitment to address this public health problem, demonstrated by the formation and work of the National Anemia Working Group (NAWG) (Sarkar and Adero 2017).
Figure 1. Steps Involved in SPRING’s MNP Costing Study
One potential intervention for reducing iron-deficiency, and therefore also the proportion of anemia that is associated to iron deficiency, in young children is providing children ages 6 to 23 months with multiple micronutrient powder (MNP) supplements; single-dose sachets of vitamins and minerals added to food every other day (Armstrong 2009; Horton 2006; Olney et al. 2012). The United States Agency for International Development’s Strengthening Partnerships, Results and Innovations in Nutrition Globally (SPRING) project carried out an MNP costing study that reported cost estimates of MNP distribution based on actual programmatic costs (from start-up costs through “last mile” of distribution to beneficiaries). The study compared the costs incurred using two delivery platforms – facility-based (“facility arm”) where caregivers receive MNP at a health facility, versus a community-based delivery channel utilizing volunteer village health team (VHT) distribution (“community arm”).
The study focused exclusively on children ages 6–23 months and was undertaken in Namutumba District, in rural Uganda. This costing research addressed three main questions:
- Which distribution method results in the best outputs of coverage1?
- Which distribution method has the most cost-efficient performance for coverage and adherence2?
- How does scaling up through different program implementation approaches affect program costs and cost-efficiency?
SPRING’s MNP study is the first reported study to assess actual costs of an MNP intervention program that permit the comparisons of costs and cost-efficiency across alternative delivery platforms (Figure 1). Since we did not measure anemia in the children participating in the pilot program, we cannot assess the effectiveness of the intervention, and hence the comparative cost-effectiveness of the two types of MNP distribution.

The detailed costs calculated for the MNP supply chain (Figure 2) included procurement of MNP packet and the transportation between storage locations and the final “last-mile” delivery to households either through a platform managed by health facilities or by volunteer VHT. Additionally, this study calculated costs for the program’s capital investments, start-up costs, capacity building, social and behavior change activities, and monitoring and evaluation (Richardson and Baker 2017). This study considered both the budgetary and opportunity costs of the program overall and for each delivery platform, with particular attention paid to the opportunity costs of individuals at health centers and in households who reallocate their time from other activities to ensure MNP distribution and consumption. These opportunity costs may have important consequences for program sustainability in the long run.
Research Findings
Costs and Cost-Efficiency of Scaling-Up MNP Distribution Programs
The findings of this MNP study are presented in brief; for further information, please refer to the SPRING citations listed in Box 4 at end of this document. Figure 3 reports the total costs and the cost categories of a three-year MNP distribution program, scaled-up throughout the district, using either a community-based or facility-based delivery platform. Both scenarios involve management and technical support provided by an international NGO. Community-based platforms were more expensive than facility-based distribution, primarily due to additional costs of the volunteer VHT, mainly the opportunity costs of the volunteers’ time. MNP product cost was only one fourth of the total cost of the program. Other important costs were capacity building and “Last Mile” opportunity and logistics costs of delivering MNP.
Table 2. MNP Pilot Supply Chain Costs


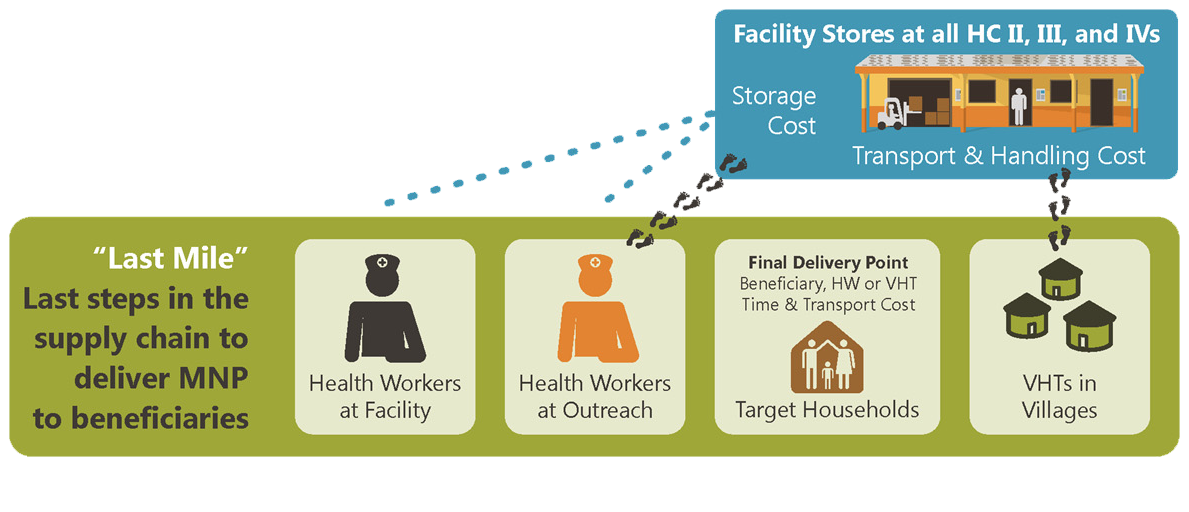
Figure 3. Cost of Implementing an MNP Program in Namutumba district, Uganda for Three Years
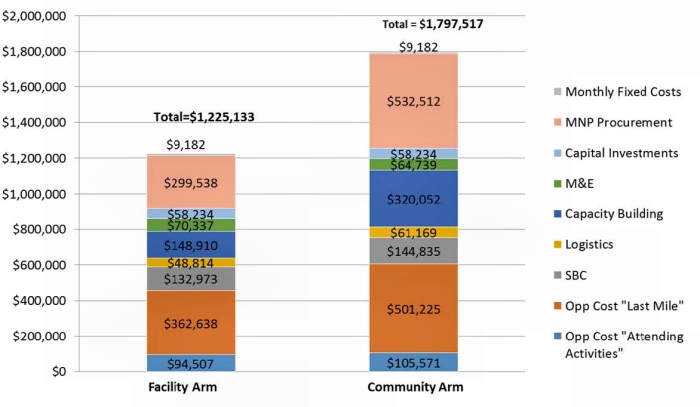
All cost data were in Ugandan shillings and converted to USD using the prevailing exchange rate.
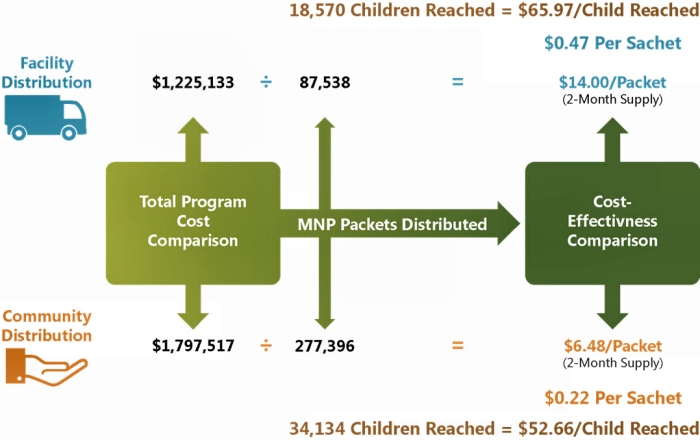
Looking only at the total program costs does not provide sufficient information for policy discussions. In the Namutumba study, even though the population sizes of young children were roughly similar in both of the study arms, the community-based platform delivered many more MNP sachets to children than the facility-based platform. Essentially, total costs were lower in the facility-based distribution mechanism because it achieved lower program coverage and reached fewer children. To obtain measures of performance, it is important to estimate cost-efficiency, which is the total cost of the programs divided by the output indicator (i.e. the total number of packets delivered and the total number of children reached). While the facility-based distribution mechanism was less costly overall, it was also less cost-effective than the community-based system to achieve best coverage (Figure 4).
Figure 4. Cost-Effectiveness of MNP Distribution Platforms in Uganda
Using the costing model developed for this study, we projected costs for alternative scale-up options based on three factors:
- management of the project (Ugandan Ministry of Health or an international NGO)
- provision (or not) of payments to volunteer VHT
- integration of MNP distribution with an existing infant and young child feeding (IYCF) public health program.
Table 1 reports the total costs and cost-efficiency (using two different criteria to qualify performance) for each of these alternative scale-up options. The selection of the output indicator greatly influences measures of cost-efficiency. From a programmatic perspective, it is important to note that the more demanding the definition of success (for example, the number of children consuming MNP according to a prescribed protocol, i.e. adherence versus the number of packets delivered), the more likely that changes in nutritional status will occur, but at a higher cost per unit of impact.
More specifically, to be effective in reducing anemia, children should be iron-deficient and they must consume MNP as recommended – one sachet mixed with food, consumed every other day. Relatively few children in either distribution platform (58 percent in community arm, 31 percent in facility arm) achieved that standard of MNP consumption, i.e. adherence to protocol. Using that metric of success, the cost/unit of averting anemia in children is much higher.
Table 1. Measures of Cost-Efficiency for Community Arm MNP Scale-Up Scenarios in Uganda
| Total Cost | Cost/Packet Distributed | Cost/Child adhered to protocol | |
|---|---|---|---|
| MOH scale-up | $1,617,804 | $5.83 | $51.70 |
| International NGO scale-up with paid VHTs | $1,680,226 | $6.06 | $53.70 |
| MOH scale-up with paid VHTs | $1,508,228 | $5.44 | $48.20 |
| International NGO integrated scale-up | $1,230,510 | $4.44 | $39.33 |
There is a subtle difference in the MOH scale-up and the international NGO integrated scale scenario – in the former, all activities are managed by the MoH; in the latter, the MNP intervention managed by an international NGO, with activities integrated into existing infant and young child feeding (IYCF) program’ activities and capital investments. For example, MNP training activities may be combined with training days for IYCF programs, and the cost of these training activities split equally between the MNP and IYCF programs. While the integrated scenario is the least expensive overall, it is important to keep in mind that integrating programs or selecting other groups to manage programs may have consequences for program quality of performance or sustainability. Furthermore, this intervention is being discussed independently of other anemia interventions. Cost-effectiveness or efficiency of MNP will need to be compared to the metrics associated with other anemia interventions, in the same context. In addition, even though we did not measure the impact of MNP on anemia, it is likely that targeted MNP interventions for particularly vulnerable populations may have greater cost-efficiency, as the effects are likely larger among those populations compared to broader interventions among the general population.

Research Recommendations
In Uganda, this study found community-based delivery platforms to be more costly overall, but they were more cost-efficient than the facility-based distribution platforms when considering the number of children reached and also children who adhered to the recommended protocol. These costs provide a reference point for policymakers in considering the costs for scale-up in districts similar in demographics and geography to Namutumba. Despite this finding, the district-wide intervention may still be too costly overall for the government to undertake. Typically, MNP are distributed in non-targeted ways – every child receives a prescribed dosage, regardless of actual need. Targeted interventions with vulnerable populations who have micronutrient deficiencies may demonstrate even more cost-favorable results.
More broadly, one costing component that is particularly salient in understanding micronutrient interventions is the unit cost of the product. Although the individual MNP sachets are inexpensive (around $0.024/sachet), there are public and private costs associated with their procurement, storage, and delivery to children, and which added represent two to three times the cost of the sachets. Another important cost to consider is the opportunity cost of volunteers, health workers, and caregivers – whose time and effort are critical to program success. The study in Uganda demonstrated that the opportunity cost for these individuals is about one-third of the total costs (as seen in the international NGO-led scale-up scenarios). While this costing study did not measure the impact of MNP on biological outcomes like anemia prevalence, we did measure the cost of performance indicators like children adhering to protocol, which were higher that cost per child reached with MNP. The sustainability of a potential MNP program in Uganda depends on linkages between performance indicators like coverage and adherence (costefficiency) and biological impact indicators like hemoglobin values (cost-effectiveness). Data on cost-efficiency and cost-effectiveness of MNP will contribute to decisions by policymakers on scaling up of MNP programs in Uganda.
Footnotes
1 We define coverage as the total number of children reached by distribution of MNP.
2 We define adherence as a caregiver reporting that a child had consumed one sachet, with food, three or more times in the past seven days.
References
Armstrong, Avril L. 2009. "Anemia in Central-Asia Pre-school Children: Definition, Risk Factors and Evaluation of Home Fortification Intervention." PhD diss., Cornell University.
Baker, Shawn K., Patrizia Fracassi, Roland Kupka, Lynette Neufeld, and Meera Shekar. 2015. "Know Your Deficiencies, Know Your Response, Know Your Costs: A Commentary on Micronutrient Program Optimization Modeling. Food and Nutrition Bulletin 36(suppl 3): S208–S210.
Belli, Pedro, ed, 2001. Economic Analysis of Investment Operations: Analytical Tools and Practical Applications. Washington, D.C.: World Bank Publications.
Engle-Stone, R., Martin Nankap, Alex O. Ndjebayi, Vosti, S. A., and Kenneth H. Brown, 2015. "Estimating the Effective Coverage of Programs to Control Vitamin a Deficiency and Its Consequences Among Women and Young Children in Cameroon. Food and Nutrition Bulletin 36(suppl 3): S149-S171.
Hendriks, Marleen E., Piyali Kundu, Alexander C. Boers, Oladimeji A. Bolarinwa, Mark J. te Pas, Tanimola M. Akande, Kayode Agbede, Gabriella B. Gomez, William K. Redekop, Constance Schultsz & Siok Swan Tan 2014. "Step-by-Step Guideline for Disease-Specific Costing Studies in Low- and Middle-Income Countries: a Mixed Methodology." Global Health Action 7:1. http://doi.org/10.3402/gha.v7.23573
Hoddinott, John. 2018. "The Investment Case for Folic Acid Fortification in Developing Countries." Annals of the New York Academy of Sciences 1414(1): 72-81.
Horton, Susan. 2006. "The Economics of Food Fortification." Journal of Nutrition 136(4): 1068–71.
Horton, Susan, Meera Shekar, Christine McDonald, Ajay Mahal, and Jana K. Brooks. 2009. Scaling up Nutrition: What Will It Cost?. Washington D.C. World Bank Publications.
Kagin, Justin, Stephen A. Vosti, Reina Engle-Stone, Erica Rettig, Kenneth H. Brown, Martin Nankap, and Alex O. Ndjebayi, A. 2015. "Measuring the Costs of Vitamin a Interventions: Institutional, Spatial, and Temporal Issues in the Context of Cameroon." Food and Nutrition Bulletin 36(suppl 3): S172-S192.
Krebs, Nancy F., Betsy Lozoff, Michael K. Georgieff. 2017. "Neurodevelopment: The Impact of Nutrition and Inflammation During Infancy in Low-Resource Settings." Pediatrics 139(Suppl 1): S50–S8.
Olney, D. K., Rawat, R., Ruel, M. T. 2012. "Identifying Potential Programs and Platforms to Deliver Multiple Micronutrient Interventions." Journal of Nutrition 142(1): 178S–85S.
Pitt, Catherine, Anna Vassall, Yot Teerawattananon, Ulla K. Griffiths, Lorna Guinness, Damian Walker, Nicola Foster, Kara Hanson. 2016. “Foreword: Health Economic Evaluations in Low- and Middle-income Countries: Methodological Issues and Challenges for Priority Setting.” Health Economics 25(Suppl 1): 1–5.
Richardson B. and Emily Baker. 2017. Cost and Cost-Effectiveness of Micronutrient Powder Distribution Pilot, Namutumba District, Uganda. Arlington, VA: SPRING.
Sarkar, Danya and Nancy Adero. 2017. Reducing Anemia in Uganda: The SPRING Approach and Lessons Learned. https://www.springnutrition.org/sites/default/files/publications/briefs/...
Uganda Bureau of Statistics (UBOS) and ICF. 2017. Uganda Demographic and Health Survey 2016: Key Indicators Report. Kampala, Uganda: UBOS and Rockville, Maryland, USA: UBOS and ICF.
Vosti, Stephen. A., Belinda Richardson, Reina Engle-Stone, and Hanqi Luo. 2017. "Understanding Factors that Influence the Benefits and Costs of Rice Fortification." In Promoción de la fortificación del arroz en América Latina y el Caribe/Scaling Up Rice Fortification in Latin America and the Caribbean, 176-182. Basel, Switzerland: Sight and Life, on behalf of the World Food Programme.
World Health Organization. 2001. Iron Deficiency Anaemia: Assessment, Prevention and Control: a Guide for Programme Managers. Geneva: WHO.
World Health Organization. 2015. The Global Prevalence of Anaemia in 2011. Geneva: WHO