Source: Irina A. Nikolic, Anderson E. Stanciole, and Mikhail Zaydman, "Chronic Emergency: Why NCDs Matter," World Bank Health, Nutrition and Population Discussion Paper (2011).
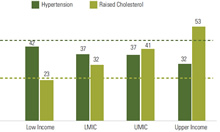
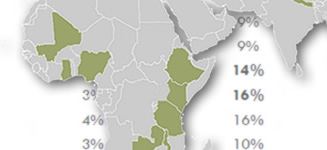
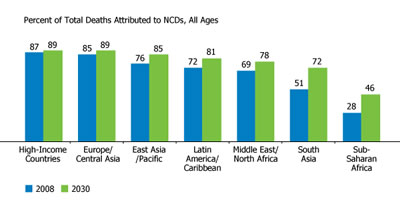
Noncommunicable diseases (NCDs) are currently responsible for over 60 percent of global deaths (World Health Organization 2012). Each year, about 80 percent of those deaths occur in low and middle income countries (LMICs;(Gersh et al. 2010)). Countries falling into this category struggle with a daunting dual burden of noncommunicable and communicable diseases, both of which require vast amounts of these countries’ limited health care resources and steal decades of productive years of life from their populations.
The resulting set of economic constraints can be crippling, both in the private and the public sectors (Gersh et al. 2010). The World Economic Forum projects that the NCD epidemic will inflict $21.3 trillion in losses in developing countries over the next two decades (Council on Foreign Relations. et al. 2014).
Over the last two decades, there has been a growing body of evidence that in-utero, infant and young child undernutrition is directly linked to vulnerability to adult nutrition-related NCD (N-RNCD;(Barker 1992; Gluckman, Hanson, and Buklijas 2010)). This suggests that health and nutrition interventions in the 1,000 days period, or from conception to two years of age, can provide additional benefits beyond the immediate term in the form of reductions in N-RNCD incidence and mortality.
USAID has asked SPRING to increase the knowledge base on the linkages between early life undernutrition interventions and their effect on later life N-RNCD outcomes. The resulting work has been able to inform where future risks may lie in low to middle income countries, the cost-effectiveness of early life N-RNCD prevention strategies, and policy and program options for incorporating N-RNCD prevention into existing country structures.
References
Barker, DJP [editor]. 1992. Fetal & Infant Origins of Adult Disease. Bmj Publishing Group.
Council on Foreign Relations., Independent Task Force on Noncommunicable Diseases, Mitchell Elias Daniels, Thomas E. Donilon, Thomas J. Bollyky, and Council on Foreign Relations. 2014. The Emerging Global Health Crisis: Noncommunicable Diseases in Low- and Middle-Income Countries. (ZIP, 9.6 MB)
De Onis, Mercedes, Adelheid W Onyango, Elaine Borghi, Cutberto Garza, Hong Yang, and WHO Multicentre Growth Reference Study Group. 2007. “Comparison of the World Health Organization (WHO) Child Growth Standards and the National Center for Health Statistics/WHO International Growth Reference: Implications for Child Health Programmes.” Public Health Nutrition 9 (07). doi:10.1017/PHN20062005.
Gersh, Bernard J, Karen Sliwa, Bongani M Mayosi, and Salim Yusuf. 2010. “Novel Therapeutic Concepts: The Epidemic of Cardiovascular Disease in the Developing World: Global Implications.”European Heart Journal 31 (6): 642–48. doi:10.1093/eurheartj/ehq030.
Gluckman, P. D., M. A. Hanson, and T. Buklijas. 2010. “A Conceptual Framework for the Developmental Origins of Health and Disease.”Journal of Developmental Origins of Health and Disease 1 (01): 6–18. doi:10.1017/S2040174409990171.